Blog & News
New SHADAC Issue Brief Highlights Lessons Learned from SIM States Working to Align Quality Measures
March 21, 2019:In an effort to improve quality and contain the growing cost of health care, states are increasingly undertaking a shift away from fee-for-service reimbursement models that reward quantity and moving toward alternative payment models that reward value.
Many of the states leading the way in payment and delivery system reform have received State Innovation Model (SIM) awards from the Center for Medicare & Medicaid Innovation (CMMI) that have aided in accelerating that work.
A new issue brief from SHADAC researcher Colin Planalp examines the work of five SIM states to develop common measure sets that align quality measures across private and public payers—a strategy aimed at reducing administrative burdens on providers and giving focus to quality improvement efforts. Drawing from the experiences of Connecticut, Massachusetts, Minnesota, Rhode Island, and Washington, the brief outlines a framework for other states to undertake quality measure alignment projects in the future.
This paper was produced by SHADAC with support from the CMMI. SHADAC is part of a team led by NORC at the University of Chicago that serves as the SIM Resource Support Contractor. SHADAC and other technical assistance partners support states and the Innovation Center in designing and testing multi-payer health system transformation approaches.
Strategy: Voluntary or Mandatory Alignment
One of the first key decisions made by states undertaking multipayer quality measure alignment is the choice between adopting a mandatory approach—requiring private payers to use the measure set—or voluntary alignment approach—encouraging stakeholder buy-in via engagement and needs prioritization. The issue brief examines both methods and highlights important considerations of each using examples of voluntary alignment from Connecticut and Washington, and examples of mandatory alignment (e.g., statutory and regulatory authorities) in Massachusetts, Minnesota, and Rhode Island.
Alignment Adoption Techniques
Each state referenced in the brief emphasized stakeholder engagement (i.e., establishing workgroups with representatives from state agencies, commercial health plans, health care providers, consumer advocates and other stakeholders) to ensure that the common measure sets met important priorities and to develop buy-in for adopting measures. The brief examines states’ stakeholder engagement strategies, as well as other techniques employed by the states to bolster their new common measure sets such as Washington’s adoption of the measures in its Medicaid and state employee health plans.
Measure Set Development: Priorities and Goals, Measure Evaluation, and Selection
The issue brief also lays out a roadmap for other states to develop their own common quality measure sets, pulling lessons from the processes employed by the five study states. The state workgroups tasked with selecting metrics for their common measure sets reported that their responsibilities generally entailed identifying and incorporating shared priorities and goals in selecting common measures, cataloguing measures currently in use within the state, selecting criteria for systematically evaluating potential measures, and evaluating and selecting measures according to those agreed-upon criteria.
Measure Set Sustainability
As a final step, the states profiled in this brief also have created and implemented processes to ensure their common measure sets will remain effective and relevant by periodically updating the measure sets by either removing measures where provider performance has topped out and/or adding new measures to address evolving quality priorities.
Lessons Learned
Ultimately, what conversations with these states revealed was a common set of lessons that can be utilized by other states planning to undertake quality measure alignment moving forward. Articulated at various points within the issue brief are recommendations for states to focus on:
- Including workgroup members from all stakeholder groups: commercial, public, state agencies, providers, consumers, and any other key groups.
- Encouraging stakeholder engagement in all aspects of selecting and implementing common measure sets.
- Strongly defining a rationale to promote stakeholder involvement, buy-in, and engagement.
- Selecting measures that are meaningful and practically applicable for providers and payers alike.
- Adopting a common measure set in public programs in order to promote mirrored alignment in commercial programs.
- Continuing to review measures after they have been set, and updating or modifying if necessary.
Read the full issue brief for more details on aligning quality measures in states.
Suggested Further Reading
Quality Measurement for HCBS and Behavioral Health in Medicaid: What’s Happening and What’s Missing
Blog & News
SHADAC Research in AJPH: Addressing Opioid Addiction through Cross-Sector Collaboration
March 5, 2019: After implementing a cross-sector collaboration between medical providers, nonmedical service providers, and a wide range of other stakeholders in the community, the town of Little Falls, Minnesota, saw a reduction in opioid use and abuse among patients at the local hospital and clinic and within the broader local rural community.
After implementing a cross-sector collaboration between medical providers, nonmedical service providers, and a wide range of other stakeholders in the community, the town of Little Falls, Minnesota, saw a reduction in opioid use and abuse among patients at the local hospital and clinic and within the broader local rural community.
In a new American Journal of Public Health article, SHADAC researchers describe the collaborative effort in Little Falls and examine results from the project.[1]
Key Components of the Intervention
The Little Falls initiative, which launched in 2014, involves two key components:
- An interdisciplinary Controlled Substance Care Team (Care Team) was established at the local hospital and clinic. The team, which consists of a social worker, a nurse, two physicians, and a pharmacist, works in consultation with any patient using a controlled substance (i.e., opioid analgesic, benzodiazepine, or stimulant) to establish a Controlled Substance Care Plan. Using this plan, the Care Team aims helps each patient to (a) taper or maintain their dosage or (b) discontinue narcotics prescriptions entirely. Importantly, the Care Team also works to address social determinants of health (e.g., housing, transportation, food access, employment) that might contribute to the overuse of controlled substances.
- The community formed a multidisciplinary task force that includes stakeholders from a range of sectors—e.g., medical, county public health and social services, law enforcement, education, etc.—in Little Falls and the surrounding area. The task force works to raise community awareness about the prevention of opioid use and abuse and facilitates community-wide collaboration on preventing and treatment prescription drug abuse. Of note, the local hospital and clinic have worked with corrections and law enforcement through their mutual task force collaboration to (a) make medication-assisted treatment available to individuals with opioid use disorder at the county jail and (b) address and reduce the diversion of prescription narcotics by hospital and clinic patients without pressing criminal charges.
Results of the Intervention
A number of results point to the success of the Little Falls initiative:
- After six months of Care Team implementation, therapeutic drug monitoring[2] went from being the top emergency department visit type at the local hospital to being absent from the top 20 visit types.
- Of the more than 1,500 clinic patients who were using controlled substances at the local hospital and clinic, 453 had been tapered off as of March 2018.
- Between January 2015 and March 2018, the local pharmacy saw a reduction of 44,952 narcotics doses prescribed each month.
- Task force law enforcement partners report that drug crimes from narcotics sales have decreased because of factors including fewer extra pills being available for diversion.
- Among 36 individuals who received MAT between May 2016 and March 2018 while incarcerated, all saw a subsequent reduction in average days incarcerated.
Learn More
Access the full article, “Addressing the Rural Opioid Addiction and Overdose Crisis through Cross Sector Collaboration: Little Falls, MN,” to learn more about the innovative collaboration efforts within the Little Falls community.
Related Reading
Minnesota’s Accountable Communities for Health: Context and Core Components
Evaluation of the Minnesota Accountable Health Model: Final Report
[1] Au-Yeung, C., Blewett, L.A., & Lange, K. (2019). “Addressing the Rural Opioid Addiction and Overdose Crisis Through Cross-Sector Collaboration: Little Falls, MN.” American Journal of Public Health, 109(2):260-262. doi: 10.2105/AJPH.2018.304789
[2] An International Classification of Diseases, Ninth Revision, code applied to many visits during which patients sought narcotics for uncontrolled pain
Blog & News
Leveraging 1332 State Innovation Waivers to Stabilize Individual Health Insurance Markets: Experiences of Alaska, Minnesota, and Oregon
February 5, 2019: A new SHADAC analysis, prepared for the Robert Wood Johnson Foundation, examines the use of 1332 State Innovations Waivers to stabilize individual health insurance markets. SHADAC researchers compared the use of this strategy in Alaska, Minnesota, and Oregon, assessing how these states navigated the 1332 waiver process; identifying lessons learned about this process and about different reinsurance models; and discussing future concerns regarding the use of reinsurance programs.
A new SHADAC analysis, prepared for the Robert Wood Johnson Foundation, examines the use of 1332 State Innovations Waivers to stabilize individual health insurance markets. SHADAC researchers compared the use of this strategy in Alaska, Minnesota, and Oregon, assessing how these states navigated the 1332 waiver process; identifying lessons learned about this process and about different reinsurance models; and discussing future concerns regarding the use of reinsurance programs.
To collect this information, SHADAC conducted an in-depth document review and qualitative interviews with 31 individuals—including state agency and executive staff, legislators, actuarial analysts, health plan representatives, program administrators, and other stakeholders—across the three study states.
Alaska, Minnesota, and Oregon: Reinsurance Models
In 2017, Alaska, Minnesota, and Oregon became the first three states to receive federal approval to establish state reinsurance programs with federal funding via section 1332 State Innovation Waivers, which authorize states to waive key ACA requirements in order to experiment with different policies in the individual and small group insurance market within certain guardrails.
- Alaska’s state reinsurance program is condition-based, paying 100% of claims from policyholders who have one of 33 possible specific medical conditions.
- The Minnesota Premium Security Plan (MPSP) is a traditional reinsurance model with an attachment point of $50,000 and a cap of $250,000 with payment of claims at an 80/20 coinsurance rate.
- The Oregon Reinsurance Program is a traditional reinsurance model with a 50/50 coinsurance rate, as well as an attachment point and cap to be determined at a later date.
Challenges and Facilitators of the 1332 Waiver Application Process
Interviewees across all stated noted numerous challenges during the 1332 waiver application process, including:
- Securing a state funding source
- Navigating rapid shifts in the political climate that affected the application process
- Being able to access timely data to support their applications
- Identifying a waivable requirement of the ACA
Respondents agreed, however, on common facilitators that aided the application process, which they listed as:
- Working hand-in-hand with insurance companies to keep them in the market
- Leveraging existing infrastructure and experience to support the state-based programs
- Using previously existing mechanisms to get analysis done quickly
- Engaging with the state’s congressional delegation
Lessons Learned about 1332 Waiver Application and Implementation Processes
Interview respondents also identified a number of lessons learned by the states as they navigated both the application and implementation stages for their 1332 waivers. A few key points are listed below.
- There are both pros and cons to condition-based vs. traditional reinsurance models.
States noted that they chose reinsurance models that would be easy to implement in a short timeframe. Traditional models were less complex, but condition-based models maximized cost of care options. - Robust communication efforts with multiple stakeholders were needed.
Respondents consistently emphasized the need for dedicated communication between state agencies, legislators, health insurers, congressional delegations, CMS officials, and community stakeholders in order to put together a successful waiver application. - Microsimulation models allowed states to be responsive to rapidly shifting policies.
States were required to submit actuarial and economic analyses as part of their waiver applications, and the microsimulation models used by Alaska and Oregon allowed them to respond to several real-time policy changes (such as the repeal of the individual mandate).
Future Concerns
Though respondents in all three states felt that state-based reinsurance was necessary to help stabilize the markets, they did report a number of concerns for the future of these programs.
- It is difficult to measure the impact of reinsurance programs beyond premium rates.
All three states reported a reduction in premium costs in the individual market as a result of implementing a reinsurance program, but other evaluations of program impacts have not been clear, often due to lack of data. - No accountability measures were included.
Due to the short turnaround time to both apply for and implement their 1332 waivers, none of the study states included accountability measures within their reinsurance programs for the individual market. - Reinsurance is only a short-term fix and does not address the underlying problem of health care costs.
Although interviewees from Alaska, Minnesota, and Oregon felt that state-based reinsurance was an important tool to stabilize the individual market, all questioned the viability of such programs as a long-term solution, commenting that individual marketplaces were only part of the whole, and only when the larger picture is addressed can the root of the issue of high health care cost be properly addressed.
Related Readings and Resources
Modeling State-based Reinsurance: One option for Stabilization of the Individual Market
Minnesota’s 13332 Reinsurance Waiver Dilemma
Resource: 1332 State Innovation Waivers for State-Based Reinsurance
Blog & News
SHADAC Releases 50-State Analysis of the Evolving Opioid Crisis (Infographics)
February 11, 2019:Much of the attention paid to the national opioid crisis in recent years has focused on the national toll of the crisis, such as the more than 44,000 opioid overdose deaths reported nationally in 2017.[1] However, the dynamics of the crisis vary widely across states, both in the prevalence of opioid overdose deaths and the types of opioids associated with those deaths.
To make state-specific information on opioid overdose deaths more easily accessible, SHADAC has used estimates from our State Health Compare online data tool to create a set of two-page infographics for all 50 states and the District of Columbia that include new data on drug overdose deaths for 2017.
Additionally, because of growing concern and evidence that the opioid crisis may be expanding to other non-opioid illicit drugs, we also have included data on drug overdose deaths from two types of drugs that are commonly involved in opioid overdoses: cocaine and psychostimulants (such as methamphetamine). [2],[3]
HIGHLIGHTS
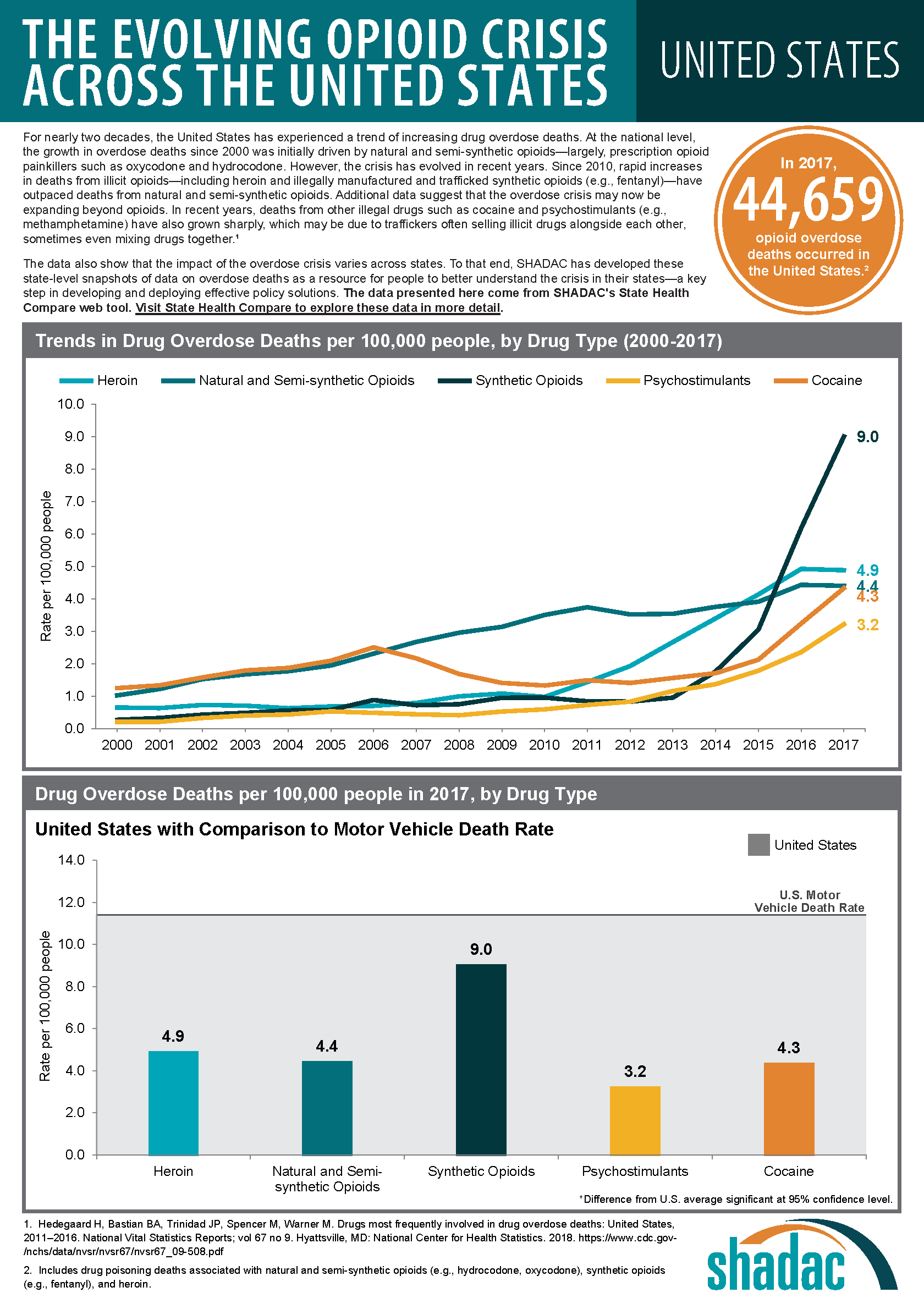
Background: U.S. trends in drug overdose deaths
At the national level, data on opioid overdose deaths show multiple, evolving phases of the overdose epidemic. From 2000 to approximately 2011, the growth in opioid overdose deaths was driven primarily by natural and semi-synthetic opioids (i.e., prescription opioid painkillers); but that death rate has since largely plateaued. Beginning around 2011, deaths from heroin began to increase more rapidly and were responsible for the highest overdose death rates in 2015. Since around 2013, however, deaths from synthetic opioids, such as fentanyl, have grown precipitously, and in 2017 the overdose death rate from synthetic opioids was nearly double the rate for all other drug types.
Around the same time that death rates from heroin and synthetic opioids began to increase, deaths from cocaine and psychostimulants also began to increase. Evidence suggests that this relationship is driven, at least in part, by an increase in deaths that involve multiple drugs. Since 2011, when deaths from heroin began to rise, death rates from cocaine have nearly tripled, from 1.5 per 100,000 people to 4.3 per 100,000 people in 2017; and death rates from psychostimulants have more than quadrupled, from 0.7 per 100,000 people to 3.2 per 100,000 people in 2017.
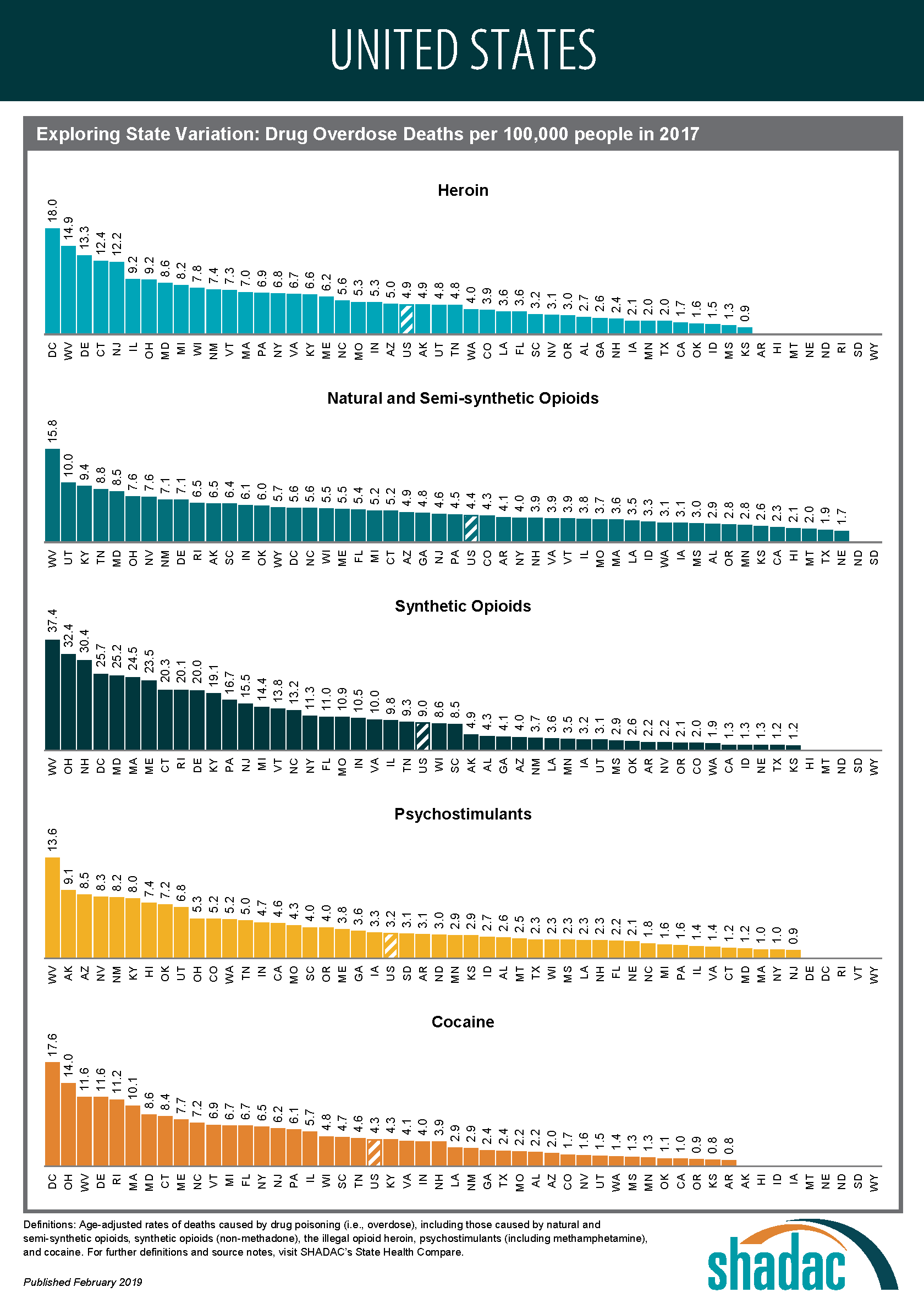
State variation in overdose deaths
Opioid Overdose Deaths
Although most states have experienced measurable increases in opioid overdose deaths since 2000, the scale of the crisis has varied widely across states. For example, West Virginia’s rate of deaths from synthetic opioids in 2017 was more than 30 times the rate of Nebraska and Texas (37.4 deaths versus 1.3 deaths per 100,000 people).
The types of opioids most commonly associated with overdoses also vary across states. For instance, Utah had the second-highest rate of deaths from natural and semi-synthetic opioids in 2017, at 10.0 deaths per 100,000 people; however, contrary to the U.S. trend, the state has experienced relatively little growth in deaths from synthetic opioids, and the state’s 2017 death rate from synthetic opioids (3.1 per 100,000 people), fell well below the U.S. rate of 9.0 per 100,000 people.
Overdose Deaths from Cocaine and Psychostimulants
The scale of overdose deaths from non-opioid illicit drugs also varies widely across states. For example, the 2017 overdose death rate from cocaine in the District of Columbia (17.6 deaths per 100,000 people) was 22 times the rate of Arkansas and Kansas (0.8 deaths per 100,000 people). Similarly, the 2017 overdose death rate from psychostimulants in West Virginia (13.6 deaths per 100,000 people) was more than 15 times the rate of 0.9 deaths per 100,000 people in New Jersey.
Regional Patterns in Drug Overdose Death Rates
Despite the evidence of state variation in drug overdose death rates, further analysis does illustrate some broader patterns:
Heroin and synthetic opioids
Death rates from heroin and synthetic opioids are generally higher east of the Mississippi River, particularly among states in the Northeast, the Appalachian region, and the industrial Midwest.
Natural and semi-synthetic opioids
Higher death rates from natural and semi-synthetic opioids are more geographically dispersed than those from heroin and synthetic opioids. While some states in the eastern U.S. have particularly high rates of deaths from natural and semi-synthetic opioids (e.g., Kentucky, Ohio, and West Virginia), there are other states in the western U.S. that also have similarly high death rates from these drugs (e.g., Utah, New Mexico, and Nevada).
Cocaine
An examination of cocaine death rates reveals a pattern similar to that of death rates from heroin and synthetic opioids, with states east of the Mississippi River exhibiting higher rates of cocaine overdose deaths.
Psychostimulants
Death rate patterns from psychostimulants appear to be almost the opposite of those for heroin and synthetic opioids, with relatively low death rates in the Northeast and particularly high rates of deaths in the western U.S. and the Southeast. Only a group of three state—Kentucky, Ohio, and West Virginia—shows strong overlaps between psychostimulant and heroin and synthetic opioid deaths.
Access the state-level infographics on drug overdose deaths.
Explore the data on drug overdose deaths on State Health Compare.
Further Reading and Resources
New Data on Drug Overdose Death Highlight the Need for State-Level Analysis
SHADAC Blog, December 2018
Exploring the New State-Level Opioid Data on SHADAC’s State Health Compare
SHADAC Webinar (Recording and Presentation Materials), September 2018
The Changing Opioid Epidemic: State Trends, 2000-2016
SHADAC Blog, August 2018
The Changing Opioid Epidemic: National Trends, 2000-2016
SHADAC Blog, July 2018
The Opioid Epidemic: National and State Trends in Opioid-Related Overdose Deaths, 2000-2016
SHADAC Issue Briefs, June 2018
[1] This number includes deaths from natural and semi-synthetic opioids (e.g., prescription opioid painkillers), heroin and synthetic opioids (e.g., fentanyl), but it excludes some opioids with relatively fewer deaths, such as methadone.
[2] Although reports of illicit drugs being tainted with synthetic opioids are relatively common, it is unclear whether deaths involving multiple drugs are typically the result of drugs being intentionally mixed by or unintentionally contaminated through traffickers’ sloppiness, or because individual drug users are concurrently abusing multiple different drugs of their own volition.
[3] U.S. Centers for Disease Control and Prevention. (2018, December 12). Drugs Most Frequently Involved in Drug Overdse Deaths: United States, 2011-2016. National Vital Stastics Report, 67(9), 1-14. Available at: https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_09-508.pdf
Publication
Leveraging 1332 State Innovation Waivers to Stabilize Individual Health Insurance Markets: Experiences of Alaska, Minnesota, and Oregon (Final Report)
 In 2017, Alaska, Minnesota, and Oregon became the first three states to receive federal approval to establish state reinsurance programs with federal funding via section 1332 State Innovation Waivers, which authorize states to waive key requirements under the law in order to experiment with different policies in the individual and small group insurance market within certain guardrails. A new SHADAC analysis, prepared for the Robert Wood Johnson Foundation, examines the use of 1332 State Innovations Waivers to stabilize individual health insurance markets within these states. SHADAC researchers compared the use of this strategy in Alaska, Minnesota, and Oregon, assessing how the 1332 waiver process was navigated; identifying lessons learned about this process and about different reinsurance models; and pinpointing future concerns about the use of reinsurance programs.
In 2017, Alaska, Minnesota, and Oregon became the first three states to receive federal approval to establish state reinsurance programs with federal funding via section 1332 State Innovation Waivers, which authorize states to waive key requirements under the law in order to experiment with different policies in the individual and small group insurance market within certain guardrails. A new SHADAC analysis, prepared for the Robert Wood Johnson Foundation, examines the use of 1332 State Innovations Waivers to stabilize individual health insurance markets within these states. SHADAC researchers compared the use of this strategy in Alaska, Minnesota, and Oregon, assessing how the 1332 waiver process was navigated; identifying lessons learned about this process and about different reinsurance models; and pinpointing future concerns about the use of reinsurance programs.
SHADAC conducted an in-depth document review and qualitative interviews with individuals - including state agency and executive staff, legislators, actuarial analysts, health plan representatives, program administrators, and other stakeholders - across the three study states who were involved in the design and/or implementation of state reinsurance programs and the 1332 waiver application process. Each of the states faced numerous challenges in their individual health insurance markets (high costs, increasing premiums, shifting marketplace makeup and plan availability, etc.) that led them to establish state-based reinsurance programs. However, as the report details, state policymakers found unique ways to facilitate both the waiver application and implementation processes, including working hand-in-hand with insurance companies, leveraging existing infrastructure and experience within their own agencies, having mechanisms in place to get analysis done quickly, and engaging with the state’s congressional delegation.
Alaska, Minnesota, and Oregon: Reinsurance Models
In 2017, Alaska, Minnesota, and Oregon became the first three states to receive federal approval to establish state reinsurance programs with federal funding via section 1332 State Innovation Waivers, which authorize states to waive key ACA requirements in order to experiment with different policies in the individual and small group insurance market within certain guardrails.
- Alaska’s state reinsurance program is condition-based, paying 100% of claims from policyholders who have one of 33 possible specific medical conditions.
- The Minnesota Premium Security Plan (MPSP) is a traditional reinsurance model with an attachment point of $50,000 and a cap of $250,000 with payment of claims at an 80/20 coinsurance rate.
- The Oregon Reinsurance Program is a traditional reinsurance model with a 50/50 coinsurance rate, as well as an attachment point and cap to be determined at a later date.
Challenges and Facilitators of the 1332 Waiver Application Process
Interviewees across all stated noted numerous challenges during the 1332 waiver application process, including:
- Securing a state funding source
- Navigating rapid shifts in the political climate that affected the application process
- Being able to access timely data to support their applications
- Identifying a waivable requirement of the ACA
Respondents agreed, however, on common facilitators that aided the application process, which they listed as:
- Working hand-in-hand with insurance companies to keep them in the market
- Leveraging existing infrastructure and experience to support the state-based programs
- Using previously existing mechanisms to get analysis done quickly
- Engaging with the state’s congressional delegation
Lessons Learned about 1332 Waiver Application and Implementation Processes
Interview respondents also identified a number of lessons learned by the states as they navigated both the application and implementation stages for their 1332 waivers. A few key points are listed below.
- There are both pros and cons to condition-based vs. traditional reinsurance models.
States noted that they chose reinsurance models that would be easy to implement in a short timeframe. Traditional models were less complex, but condition-based models maximized cost of care options. - Robust communication efforts with multiple stakeholders were needed.
Respondents consistently emphasized the need for dedicated communication between state agencies, legislators, health insurers, congressional delegations, CMS officials, and community stakeholders in order to put together a successful waiver application. - Microsimulation models allowed states to be responsive to rapidly shifting policies.
States were required to submit actuarial and economic analyses as part of their waiver applications, and the microsimulation models used by Alaska and Oregon allowed them to respond to several real-time policy changes (such as the repeal of the individual mandate).
Future Concerns
Though respondents in all three states felt that state-based reinsurance was necessary to help stabilize the markets, they did report a number of concerns for the future of these programs.
- It is difficult to measure the impact of reinsurance programs beyond premium rates.
All three states reported a reduction in premium costs in the individual market as a result of implementing a reinsurance program, but other evaluations of program impacts have not been clear, often due to lack of data. - No accountability measures were included.
Due to the short turnaround time to both apply for and implement their 1332 waivers, none of the study states included accountability measures within their reinsurance programs for the individual market. - Reinsurance is only a short-term fix and does not address the underlying problem of health care costs.
Although interviewees from Alaska, Minnesota, and Oregon felt that state-based reinsurance was an important tool to stabilize the individual market, all questioned the viability of such programs as a long-term solution, commenting that individual marketplaces were only part of the whole, and only when the larger picture is addressed can the root of the issue of high health care cost be properly addressed.
Related Readings and Resources
Modeling State-based Reinsurance: One option for Stabilization of the Individual Market
Minnesota’s 13332 Reinsurance Waiver Dilemma
Resource: 1332 State Innovation Waivers for State-Based Reinsurance