Publication
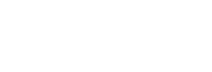
2018 State-level Estimates of Medical Out-of-Pocket Spending for Individuals with Employer-sponsored Insurance Coverage
 U.S. health care spending continues to grow, reaching $3.6 trillion and 17.7% of the GDP in 2018.[i] Unfortunately, a significant share of these costs are increasingly born by Americans in the form of increased deductibles, copayment, and coinsurance—commonly referred to as patient “out-of-pocket” (OOP) costs. Even for the 52% of Americans who have private health insurance through their own or their spouse’s employer, affordability of health care is a pressing issue. Nationally, the average deductible for families in 2018 was $3,392, and almost half (49.1%) of all Americans were enrolled in high-deductible health plans with a deductible of at least $2,700 for family coverage.[ii],[iii]
U.S. health care spending continues to grow, reaching $3.6 trillion and 17.7% of the GDP in 2018.[i] Unfortunately, a significant share of these costs are increasingly born by Americans in the form of increased deductibles, copayment, and coinsurance—commonly referred to as patient “out-of-pocket” (OOP) costs. Even for the 52% of Americans who have private health insurance through their own or their spouse’s employer, affordability of health care is a pressing issue. Nationally, the average deductible for families in 2018 was $3,392, and almost half (49.1%) of all Americans were enrolled in high-deductible health plans with a deductible of at least $2,700 for family coverage.[ii],[iii]
The State Health Access Data Assistance Center (SHADAC) at the University of Minnesota continues to monitor trends in coverage, access, and affordability. This brief highlights the affordability of coverage for those with employer-sponsored health insurance (ESI). Using data from the Annual Social and Economic Supplement (ASEC) of the 2019 Current Population Survey (CPS; data year 2018), we estimated family out-of-pocket costs for people with employer coverage across all 50 states and the District of Columbia (D.C.). For individuals with ESI, we looked at: (1) the family median out-of-pocket costs by state, and (2) an estimate of the high medical cost burden where family out-of-pocket spending is greater than 10% of household income. For additional estimates, please visit SHADAC’s State Health Compare web tool.
[i] Centers for Medicare & Medicaid Services (CMS). (2019, December 5). NHE Fact Sheet. Retrieved from https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet/
[ii] State Health Access Data Assistance Center analysis of the 2018 American Community Survey microdata.
[iii] State Health Access Data Assistance Center, State-level Trends in Employer-Sponsored Health Insurance, 2014-2018. Available at: https://www.shadac.org/ESIReport2019
Blog & News
Affordability and Access to Care in 2018: Examining Racial and Educational Inequities across the United States (Infographic)
December 17, 2019: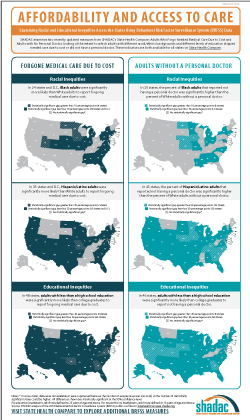 The Centers for Medicare and Medicaid Services (CMS) recently reported that the cost of health care spending in the United States increased by 4.6 percent last year to reach an all-time high of approximately $3.6 trillion.1 This report comes amidst a number of other concerning health care cost-related trends, such as the largest single-year increase for single-coverage premiums in 2018 from $6,368 to $6,715 (5.4 percent) for workers enrolled in employer-sponsored insurance (ESI) and an increase in average household spending on health care (out of pocket expenses, cost-sharing for ESI, and payroll taxes for Medicare, etc.) rising to a record $1.04 trillion.2
The Centers for Medicare and Medicaid Services (CMS) recently reported that the cost of health care spending in the United States increased by 4.6 percent last year to reach an all-time high of approximately $3.6 trillion.1 This report comes amidst a number of other concerning health care cost-related trends, such as the largest single-year increase for single-coverage premiums in 2018 from $6,368 to $6,715 (5.4 percent) for workers enrolled in employer-sponsored insurance (ESI) and an increase in average household spending on health care (out of pocket expenses, cost-sharing for ESI, and payroll taxes for Medicare, etc.) rising to a record $1.04 trillion.2
Rising expenses such as these have contributed to the record number of Americans (25 percent) who reported in 2019 that either themselves or a family member skipped or delayed needed medical care due to cost, according to the results from a new Gallup poll released earlier this month.3
This post examines Americans’ access and ability to afford medical care, focusing on inequities related to race/ethnicity and education, and using two recently updated measures from SHADAC’s State Health Compare: Adults Who Forgo Needed Medical Care and Adults with No Personal Doctor. These measures come from a SHADAC analysis of 2018 data from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS).
Racial and educational inequities persist in adults’ reported ability to afford needed medical care
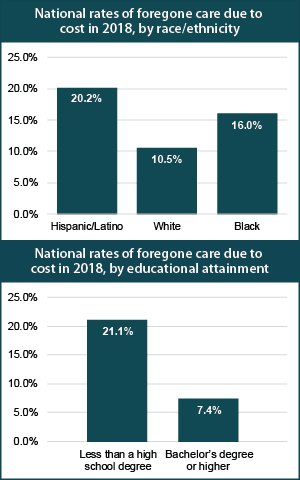 Significant inequities in adults’ ability to afford medical care by race/ethnicity emerged when we examined the updated data for 2018. At the national level, our analysis showed that Hispanic/Latino adults were nearly twice as likely as White adults to forgo needed medical care due to cost (20.2 percent versus 10.5 percent), and African Americans/Black adults were 1.5 times as likely to report forgoing care compared to White adults (16.0 percent versus 10.5 percent). Hispanic/Latino adults were also significantly more likely to report forgoing medical care than White adults in 35 states and D.C., and this gap was greater than 20 percentage points in Maryland (31.4 percent versus 7.4 percent) and Missouri (34.4 percent versus 11.1 percent). Black adults were significantly more likely to report going without care than White adults in 24 states and D.C., and this gap was greater than 10 percentage points in four states: Iowa (16.2 percentage points), North Dakota (15.5 percentage points), Utah (11.5 percentage points), and Minnesota (10.2 percentage points).
Significant inequities in adults’ ability to afford medical care by race/ethnicity emerged when we examined the updated data for 2018. At the national level, our analysis showed that Hispanic/Latino adults were nearly twice as likely as White adults to forgo needed medical care due to cost (20.2 percent versus 10.5 percent), and African Americans/Black adults were 1.5 times as likely to report forgoing care compared to White adults (16.0 percent versus 10.5 percent). Hispanic/Latino adults were also significantly more likely to report forgoing medical care than White adults in 35 states and D.C., and this gap was greater than 20 percentage points in Maryland (31.4 percent versus 7.4 percent) and Missouri (34.4 percent versus 11.1 percent). Black adults were significantly more likely to report going without care than White adults in 24 states and D.C., and this gap was greater than 10 percentage points in four states: Iowa (16.2 percentage points), North Dakota (15.5 percentage points), Utah (11.5 percentage points), and Minnesota (10.2 percentage points).
Nationwide, Americans with less than a high school degree were almost three times as likely to report going without needed medical care due to cost as compared to those with a bachelor’s degree (21.1 percent versus 7.4 percent) in 2018. Adults with less than a high school education were significantly more likely to report forgone care due to cost compared to adults with college degrees in 2018 in all but two states—Montana and Vermont—and in the District of Columbia (D.C.). For four states this gap was greater than 20 percentage points in 2018—Georgia (21.1 percentage points), Maryland (20.9 percentage points), Oklahoma (21.2 percentage points), and Virginia (21.2 percentage points).*
Racial/ethnic minorities and adults without a high school diploma less likely to have a personal doctor
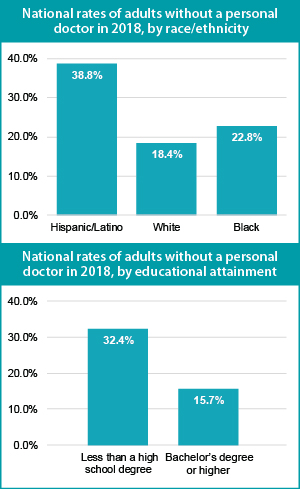 Nationally, Hispanic/Latino and Black adults were both significantly more likely to report not having a regular doctor as compared to their White counterparts. Our analysis revealed that Hispanic/Latino adults were more than twice as likely as White adults to report not having a personal doctor (38.8 percent versus 18.4 percent), and Black adults were nearly 25 percent more likely to report not having a personal doctor compared with White adults (22.8 percent versus 18.4 percent).*
Nationally, Hispanic/Latino and Black adults were both significantly more likely to report not having a regular doctor as compared to their White counterparts. Our analysis revealed that Hispanic/Latino adults were more than twice as likely as White adults to report not having a personal doctor (38.8 percent versus 18.4 percent), and Black adults were nearly 25 percent more likely to report not having a personal doctor compared with White adults (22.8 percent versus 18.4 percent).*
These inequities in access to care by race/ethnicity were present in a large majority of states. A significant gap between Hispanic/Latino and White adults with no personal doctor was present in 43 states, and Hispanic adults were more than three times as likely to report not having a personal doctor in five states (Connecticut, Maryland, Nebraska, New Jersey, and North Carolina). This significant gap also persisted between Black and White adults in 20 states, as we found that Black adults were more than twice as likely to not have a personal doctor in three states—Connecticut (22.8 percent versus 10.8 percent), Iowa (31.2 percent versus 15.1 percent), and Rhode Island (21.2 percent versus 9.9 percent).*
Nationally, adults with less than a high school degree were more than twice as likely to not have a regular doctor as those with an undergraduate degree or greater (32.4 percent versus 15.7 percent). This pattern was consistent across nearly the entire nation, as adults with less than a high school education were significantly more likely than college graduates to report not having a personal doctor in 46 states. The gap between less than high school graduates and college graduates was larger than 20 percentage points in eight states (California, Colorado, Georgia, Maryland, Nebraska, Nevada, New Jersey, and Utah).
Note
* Data were not available or were suppressed for some states because the number of sample cases was too small, so this number could be higher if data were available in all states. For education breakdowns, adults are defined as 25 years of age and above. For race/ethnicity breakdowns, adults are defined as 18 years of age and above. All differences are statistically significant at the 95% level.
Explore Additional BRFSS Data at State Health Compare
Visit State Health Compare to explore national and state-level estimates for the following measures that also come from the BRFSS:
Income Inequality
Sales of Opioid Painkillers
Adult Cancer Screenings
Chronic Disease Prevalence
Activities Limited due to Health Difficulty
Adult Obesity
Adult Binge Drinking
Adult Smoking
Adult E-Cigarette Use (New Measure)
State Health Compare also features a number of other indicator categories, including: health insurance coverage, cost of care, access to and utilization of care, care quality, health behaviors, health outcomes, and social determinants of health.
Related Reading
Now Available on State Health Compare: Eleven Updated Measures and One Brand New Measure
Educational Attainment and Access to Health Care: 50-State Analysis
Fifty-State Analysis Finds Lower Access to Care among Adults with Less Education
[1] Hartman, M., Martin, A.B., Benson, J., & Catlin, A. (2019, December 5). National Health Care Spending in 2018: Growth Driven by Accelerations in Medicare and Private Insurance Spending. HealthAffairs. [E-published ahead of print.] https://doi.org/10.1377/hlthaff.2019.01451
[2] State Health Access Data Assistance Center (SHADAC). (2019, August 14). State-level Trends in Employer-Sponsored Health Insurance, 2014-2018. Retrieved from https://www.shadac.org/ESIReport2019
Murad, Y. (2019, December 5). U.S Health Spending Rose to $3.6 Trillion in 2018, Propelled by Health Insurance Tax. Morning Consult. Retrieved from https://morningconsult.com/2019/12/05/u-s-health-spending-rose-to-3-6-trillion-in-2018-propelled-by-health-insurance-tax/
[3] Saad, L. (2019, December 9, 2019). More Americans Delaying Medical Treatment Due to Cost. Retrieved from https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx
Blog & News
Now Available on State Health Compare: Eleven Updated Measures and One Brand New Measure
December 3, 2019:Estimates for measures from a variety of categories (Health Outcomes, Health Behaviors, Access to Care, Cost of Care, and Social and Economic Factors, etc.) have now been updated on SHADAC’s State Health Compare web tool. All measures now contain data for 2018, the most recent year available. State Health Compare has also added a brand new measure, Adult E-Cigarette Use.
Updated Measures Include:
Income Inequality
Using the Gini coefficient (a summary of the dispersion of income across the entire income distribution), this measure gauges disparities in income in each state on a scale from 0 to 1, with higher values indicating greater inequality and lower values indicating the opposite. Estimates for all states are now available from 2006 through 2018.
Sales of Opioid Painkillers
This measure captures the rate of legal prescription opioid painkiller sales in kilograms per 100,000 people per year for both hydrocodone and oxycodone—the most common types of prescription opioids. Data is now available for all states from 2000 through 2018.
Adults Who Forgo Needed Medical Care*
The measure indicates the percent of adults (18+) in each state who could not get needed medical care due to cost. Breakdowns by education level and race/ethnicity are available for all states from 2005 through 2010 and 2011 through 2018.
Adults With No Personal Doctor*
This measure denotes the percent of adults without a personal doctor and is now available for all states from 2005 through 2010 and 2011 through 2018. Breakdowns by education level and race/ethnicity are also available.
Adult Cancer Screenings*
The measure is an indication of the percent of adults who have received recommended cancer screenings (e.g., colorectal screenings, mammograms, pap smears, etc.) in the past year, and is now available for all states from 2005 through 2010 and 2011 through 2018.
Chronic Disease Prevalence*
This measure captures the percent of adults who reported having one or more common chronic conditions such as diabetes, cardiovascular disease, heart attack, stroke, and asthma, in each state. Estimates are now available for all states from 2005 through 2010 and 2011 through 2018.
Activities Limited due to Health Difficulty*
This measure reports the average number of days (in the last 30 days) for which an adult indicates limited activity due to mental or physical health difficulties. It is now available for all states from 2005 through 2010 and 2011 through 2018.
Adult Obesity*
The measure is an indication of the prevalence of obesity, defined as a Body Mass Index (BMI) > 30, among the adult population 18 years of age and over. It is now available for all states from 2005 through 2010 and 2011 through 2018.
Adult Binge Drinking*
This measure indicates the percent of adults who, on one occasion, have consumed at least four drinks (women) or five (men) or more in the past 30 days. Now available for all states from 2005 through 2010 and 2011 through 2018, the measure includes breakdowns by education level and race/ethnicity.
Adult Smoking*
This measure indicates the percent of adults over 18 years of age who have smoked 100 or more cigarettes in their lifetime, and who currently smoke some days or every day. It is now available for all states from 2005 through 2010, and 2011 through 2018.
Adult E-Cigarette Use (Newly available measure on State Health Compare)
This measure indicates the percent of the adult population (18 years of age and over) who currently use e-cigarette some days or every day. It is now available for all states from 2016 through 2017 and for most states for 2018. Breakdowns are available by education level and race/ethnicity.
Data Sources
The State Health Compare estimates for income inequality come from the American Community Survey (ACS); the sales of opioid painkillers comes from the U.S. DEA’s Automated Reports Consolidated Ordering System Retail Drug Summary Reports; and the measures of chronic disease prevalence, activities limited due to health difficulty, and the adults who forgo needed medical care, adults with no personal doctor, and adult cancer screenings, obesity, binge drinking, smoking, and e-cigarette use measures all come from the Behavior Risk Factor Surveillance System (BRFSS).
Notes
All measures marked with an “*”: This indicates a break in series due to the BRFSS implementing cell phone sampling and an advanced weighting method in 2011.
SHADAC Expertise
Health Coverage and Access to Care
Since its inception, SHADAC has been dedicated to conducting research and providing technical assistance in order to examine characteristics of and trends in health insurance coverage and access to care and associations with overall physical, social, and mental health status. Our work on these topics includes technical briefs describing the complexity of measuring health insurance coverage and understanding the strengths and weaknesses of various data sources, e.g., federal and state-specific surveys, towards the goal of improving estimates of health insurance coverage, which is critical to the evaluation of federal and state health reform efforts. We also have conducted research studies of access to care during the coronavirus pandemic, insurance churning in Medicaid, and insurance-based discrimination. We have helped states field their own health insurance surveys or used federal data to help states target their coverage-related efforts as well as produced 50-state analyses of geographic disparities in coverage and key measures of health care access with data from State Health Compare.
Related SHADAC work
Click on any title below to learn more about the project.
Disparities in Access to Care During the Pandemic in California
This data brief examines whether and how access to care shifted during the pandemic for people with Medi-Cal, compared to those with employer coverage. Researchers compared data from the 2017–18 and 2020–21 California Health Interview Survey (CHIS). Data show that the pandemic did not widen differences in access to care for people with Medi-Cal coverage compared to those with employer coverage. among adults, there was some narrowing of differences on select measures. However, this is not a positive development, as it appears to have been caused by worsening access to care for adults with employer-sponsored insurance coverage during the pandemic rather than improvements for adults with Medi-Cal.
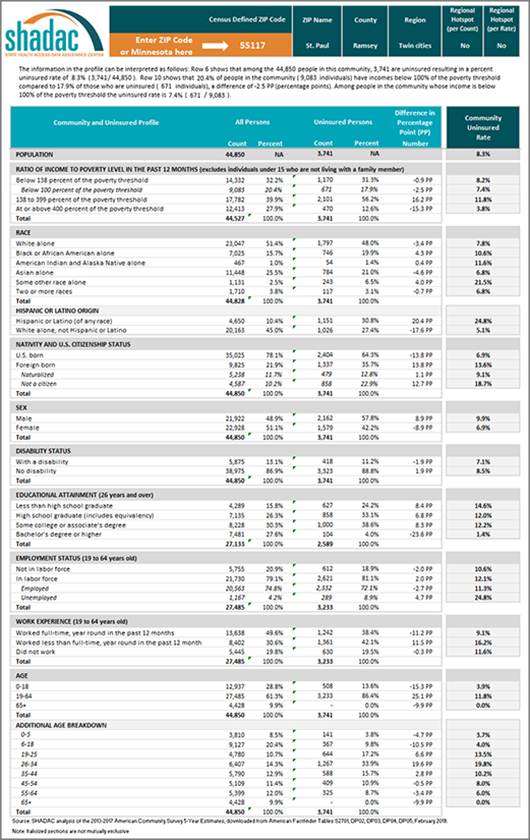
Minnesota’s Community and Uninsured Profile
The Community and Uninsured Profile provides rates and counts of Minnesotans at a range of geographic levels using data from the American Community Survey (ACS). This resource was originally developed as part of “Minnesota’s Uninsured and the Communities in Which They Live,” a project funded by the Blue Cross Blue Shield Foundation of Minnesota that supports targeted outreach and enrollment activities of health insurance navigators and provides information about the uninsured to Minnesota policymakers as they develop strategies to reach the remaining uninsured in Minnesota. Users can explore characteristics of the total population and the uninsured population in a specific ZIP code while also overlaying in-depth community characteristics. In addition, users can look at rates and characteristics of the community and uninsured within the state as a whole, by region, county, and state legislative district. Users can also filter by MNsure rating areas -- the geographic regions health insurers use to set premiums on MNsure. You can also case studies highlighting how the profile can support the enrollment efforts of local organizations and departments in our blog on the topic here.
Telehealth Use and Experiences Among California Adults
This California Health Care Foundation (CHCF) issue brief authored by SHADAC's Senior Research Fellow Lacey Hartman uses data from the 2021 California Health Interview Survey (CHIS) to explore how telehealth use varies across subpopulations of adults in the state and reports how people rate their telehealth experience compared to in-person care. The brief concludes with a discussion of potential policy implications of the findings, and areas for future data collection and research.
Examining Gender-Based Discrimination in Health Care Access by Gender Identity in Minnesota
The biennial 2021 Minnesota Health Access Survey (MNHA) asked respondents how often their gender, sexual orientation, gender identity, or gender expression causes health care providers to treat them unfairly. We compared rates of gender-based discrimination and health care access in the Minnesota adult population and examined differences in access to care among cisgender (cis) and gender minorities who report gender-based discrimination. We explored the impact of gender-based discrimination on health care access by comparing access rates among people who did and did not experience discrimination for cis men, cis women, transgender and non-binary populations in Minnesota. Click on the title above to learn more, and read more on Sexual Orientation and Gender Identity (SOGI) discrimination in our blog here where we further examine 2021 MNHA data.
Minnesota Health Access (MNHA) Survey
The Minnesota Health Access (MNHA) Survey, conducted collaboratively between SHADAC and the Minnesota Department of Health (MDH), is a large-scale telephone and mail survey that collects information on the health of Minnesotans and how they access health insurance and health care services. The survey is conducted every two years and results are presented in a follow-up report from MDH.
Past Work
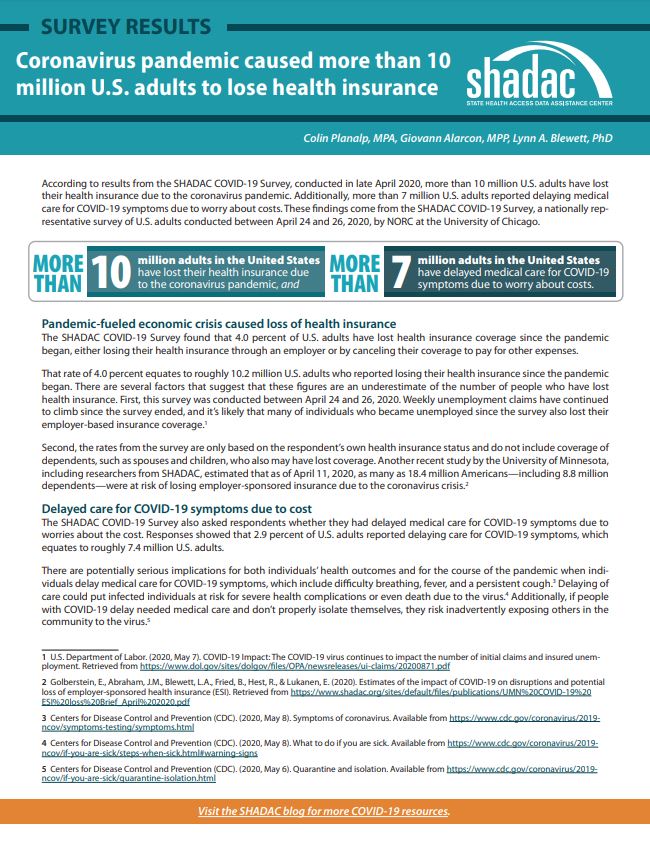
Reduced Access to Health Care due to Coronavirus Pandemic - SHADAC COVID-19 Survey
SHADAC conducted a two-part survey initially designed to measure the impacts of the novel coronavirus on a variety of experiences for adults in the United States. The survey was conducted as part of the AmeriSpeak omnibus survey conducted by NORC at the University of Chicago using a mix of phone and online modes among a nationally representative sample of 1,007 respondents age 18 and older. The first iteration of the survey was fielded in late April 2020, and questions focused on health insurance coverage, access to and cost of care during the pandemic, as well as COVID-related stressors and coping mechanisms. A second version of the survey was again fielded in April of 2021, with questions aimed at understanding respondents’ experiences with illness and death due to COVID-19 for themselves, their families, and their contacts. A collective list of products we have produced using results from the SHADAC COVID-19 Survey can be found here.
Impacts of the Affordable Care Act Medicaid Expansion in California
With funding from the California Health Care Foundation, SHADAC conducted an analysis of the impact of the Medicaid expansion on healthcare coverage, access, health status, affordability, and disparities in these outcomes by race/ethnicity for low-income Californians. Researchers on this project used nationally representative survey data from the Behavioral Risk Factor Surveillance Survey (BRFSS) 2011-2019 data years and a difference-in-differences approach that compared California with non-expansion states.
MACPAC Analysis of Insurance Churning
SHADAC conducted a quantitative analysis for MACPAC that explored the magnitude and type of churn among the Medicaid population. Specifically, the study used the Survey of Income and Program Participation Panel (SIPP) to examine the characteristics of those who churned with those who had continuous Medicaid coverage throughout the year and explored possible causes of churn. The study produced descriptive statistics to address many of the research questions and regression analysis to explore life events that potentially cause churn. The study team was able to produce state-level estimates by leveraging the large sample size of the American Community Survey (ACS) to enhance the statistical power of the SIPP by post stratifying the individual weights to match a variety of relevant population estimates in the ACS.
The Intersection of Structural Risk Factors and Insurance-based Discrimination on Healthcare Access Inequities
Social risk factors independently influence experiences of discrimination and they converge leaving some people even more vulnerable leading to worse access to healthcare. Supported by a grant from the Robert Wood Johnson Foundation (RWJF) and in collaboration with the Minnesota of Department of Health and Minnesota Department of Human Services, researchers conducted an evaluation on the effects of insurance-based discrimination and other social risk factors (e.g., low income, minority status) on disparities in access to healthcare services.
Blog & News
New SHADAC Brief Explores National and State Estimates of Gains in Equitable Coverage for Mental Health and Substance Use Disorder under the ACA
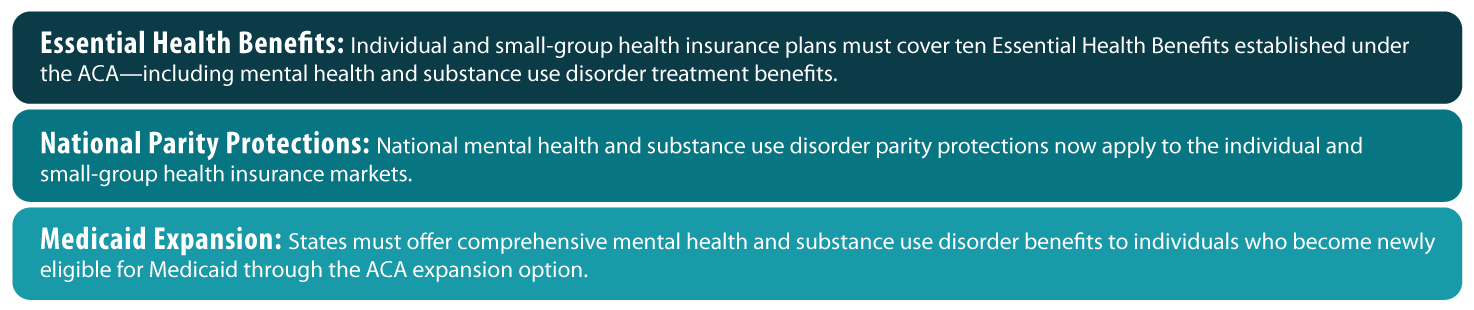
July 09, 2019: A new brief from SHADAC, supported by the California Health Care Foundation (CHCF), examines gains in equitable coverage (i.e., “parity”) for mental health and substance use disorder (MH/SUD) treatment for people in the individual and small-group markets as well as those covered under Medicaid expansion after the passage of the Affordable Care Act (ACA). National and state-level estimates of parity gains for both types of treatment are provided within the brief, and estimates are broken down for the individual market, the small-group market, and the Medicaid expansion population.[1] These estimates provide important context for policymakers and others engaged in the ongoing debate about repealing, modifying, or replacing the ACA.
A new brief from SHADAC, supported by the California Health Care Foundation (CHCF), examines gains in equitable coverage (i.e., “parity”) for mental health and substance use disorder (MH/SUD) treatment for people in the individual and small-group markets as well as those covered under Medicaid expansion after the passage of the Affordable Care Act (ACA). National and state-level estimates of parity gains for both types of treatment are provided within the brief, and estimates are broken down for the individual market, the small-group market, and the Medicaid expansion population.[1] These estimates provide important context for policymakers and others engaged in the ongoing debate about repealing, modifying, or replacing the ACA.
Background
Before the ACA, national legislation regarding equitable coverage for MH/SUD treatments applied only to large-group (i.e., employer-sponsored) health plans, as a result of the Mental Health Parity Act of 1996 (MHPA) and the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA). The ACA extended these MH/SUD parity protections beyond the large-group market to the individual and small-group markets and to Medicaid expansion beneficiaries by making MH/SUD treatments an essential health benefit (EHB). Before this change, coverage and parity for MH/ SUD treatment in these markets were addressed unevenly across states through a patchwork of state laws.
Expanding Equitable Coverage of Mental Health and Substance Use Disorder Treatment under the ACA: Key Provisions
Findings
Mental Health
In total, an estimated 39 million individuals nationwide had health insurance that was subject to the ACA’s expanded MH parity requirements as of 2017. Of these, 12.1 million were enrolled in individual plans, 14.4 million were enrolled in small-group plans, and almost 13 million were newly eligible Medicaid expansion enrollees.
At the state level, California saw the greatest number of individuals affected at approximately 8.6 million. Other states that had high estimates of affected populations included New York with 2.1 million, Florida with 2.08 million*, Texas with 1.9 million*, and Pennsylvania with 1.87 million.
Vermont, which had pre-ACA parity in both the individual and small-group market and had expanded Medicaid in advance of the ACA, was the only state that saw no effect. Other states such as Wyoming*, Alaska, and Delaware, all had affected populations of less than 100,000 (44,000; 67,000; and 80,000, respectively).
Substance Use Disorder
In total, an estimated 36.4 million individuals nationwide had health insurance that was subject to the ACA’s expanded SUD parity requirements as of 2017. Of these, 9.8 million were enrolled in individual plans, 14 million were enrolled in small-group plans, and almost 12 million were newly eligible Medicaid expansion enrollees.
At the state level, California saw the greatest number of individuals affected at approximately 8.26 million, followed by New York (2.09 million), Florida* (1.79 million), Pennsylvania (1.79 million) and Texas* (1.7 million).
Massachusetts, which had pre-ACA parity in both the individual and small-group market and had expanded Medicaid in advance of the ACA, was the only state that saw no effect. Other states such as Delaware, Wyoming*, Maine*, and Alaska all had affected populations of less than 100,000 (12,000; 39,000; 52,000; and 64,000, respectively).
Discussion
Though the ACA mandated access to health insurance coverage with parity for treatment of mental health and substance use disorders for new groups, it is important to note that the expansion of coverage parity legislation does not guarantee access to equitable MH/SUD services unless the legislation is enforced. Responsibility for parity enforcement falls primarily to states, and the nature and extent of enforcement is consequently inconsistent across the country, with many parity violations continuing to occur as state regulators face limitations in their enforcement capacities.
Further Reading
Access and Cost Barriers to Mental Health Care, by Insurance Status, 1999-2010
Kathleen Rowan, Donna McAlpine, and Lynn Blewett
Section 1115 Waivers and ACA Medicaid Expansions: A Review of Policies and Evidence from Five States: May 2016
SHADAC Special Issue Brief
Medicaid Expansion: Comparing State Choices in Alternative Benefit Plan Design
Colin Planalp
To learn more about mental health and state-level estimates for the affected population who report mentally unhealthy days, see our recent blog post, and visit State Health Compare to learn more about the measure and its data sources.
[1] National estimates do not include a Medicaid expansion breakdown because expansion has only occurred at the state level.
* No Medicaid expansion