Blog & News
Since the ACA, High-Burden Health Spending Declined among Individual-Market and Medicare Beneficiaries
April 24, 2017:A new SHADAC analysis shows a statistically significant decline in high-burden health care spending among people with individual-market coverage since the 2014 implementation of the Affordable Care Act (ACA). These and other findings are described in a new brief, funded by the California Health Care Foundation, that examines changes in U.S.- and state-level measures of financial burden and cost-related barriers to care since implementation of the ACA.
Between 2013 and 2015, there was a statistically significant 5.9 percentage point decline (from 44.7% to 38.8%) in the U.S. rate of people with individual-market coverage who reported spending more than 10% of family income on out-of-pocket (OOP) health costs. This includes spending such as insurance premiums, deductibles, co-pays and spending on prescription drugs. Average OOP spending among people with individual-market coverage also declined significantly from $6,831 to $5,508 over the same time period.
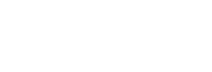
Five states experienced statistically significant declines (see Table 1 below) in high-burden spending for people with individual-market coverage (Oklahoma was the only state to see a significant increase.) These improvements likely resulted from the ACA’s financial assistance designed to make individual-market health insurance more affordable, such as advanced premium tax credits to reduce monthly premiums and cost-sharing subsidies to reduce people’s spending on deductibles, co-pays and certain other costs.
Table 1: Statistically Significant Changes in Individual-market High-burden Health Spending, 2013 & 2015 (all ages)
While these changes are positive, it will be important to continue tracking high-burden spending among people with individual-market coverage to see whether the improvements continue. Because the American Health Care Act—which would have repealed and replaced some parts of the ACA—was not passed in March 2017, the ACA’s advanced premium tax credits are expected to continue as currently implemented, as least in the near term. However, it is not assured that high-burden health spending will continue to decline, or even that the current reductions will be maintained. A pending lawsuit could result in the cancelation of cost-sharing subsidies, which would increase OOP costs for some lower-income people with individual-market coverage, and other proposals to reduce or eliminate premium tax credits could resurface in the future.[i]
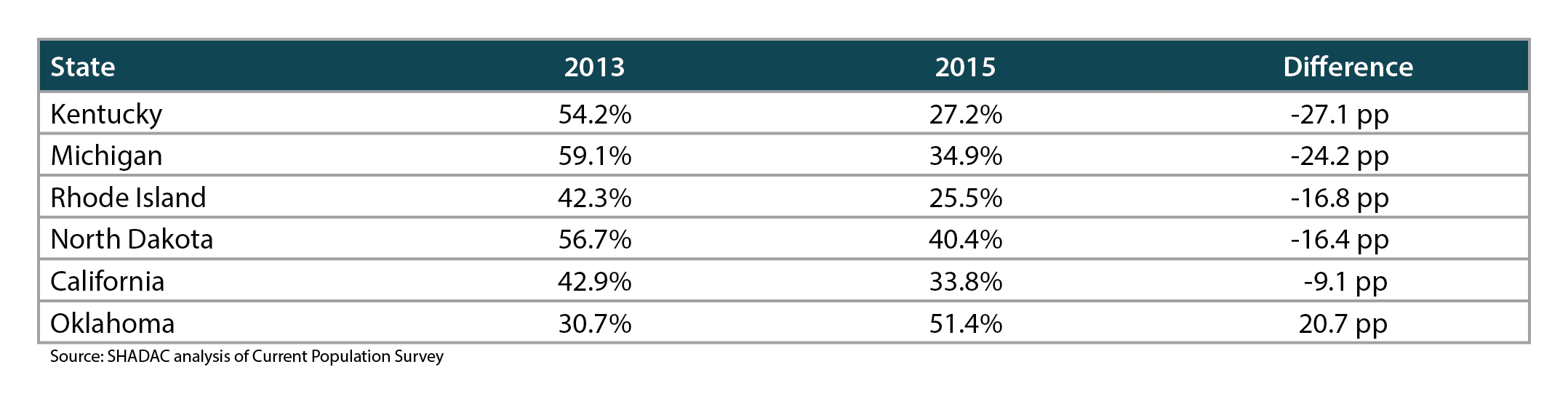
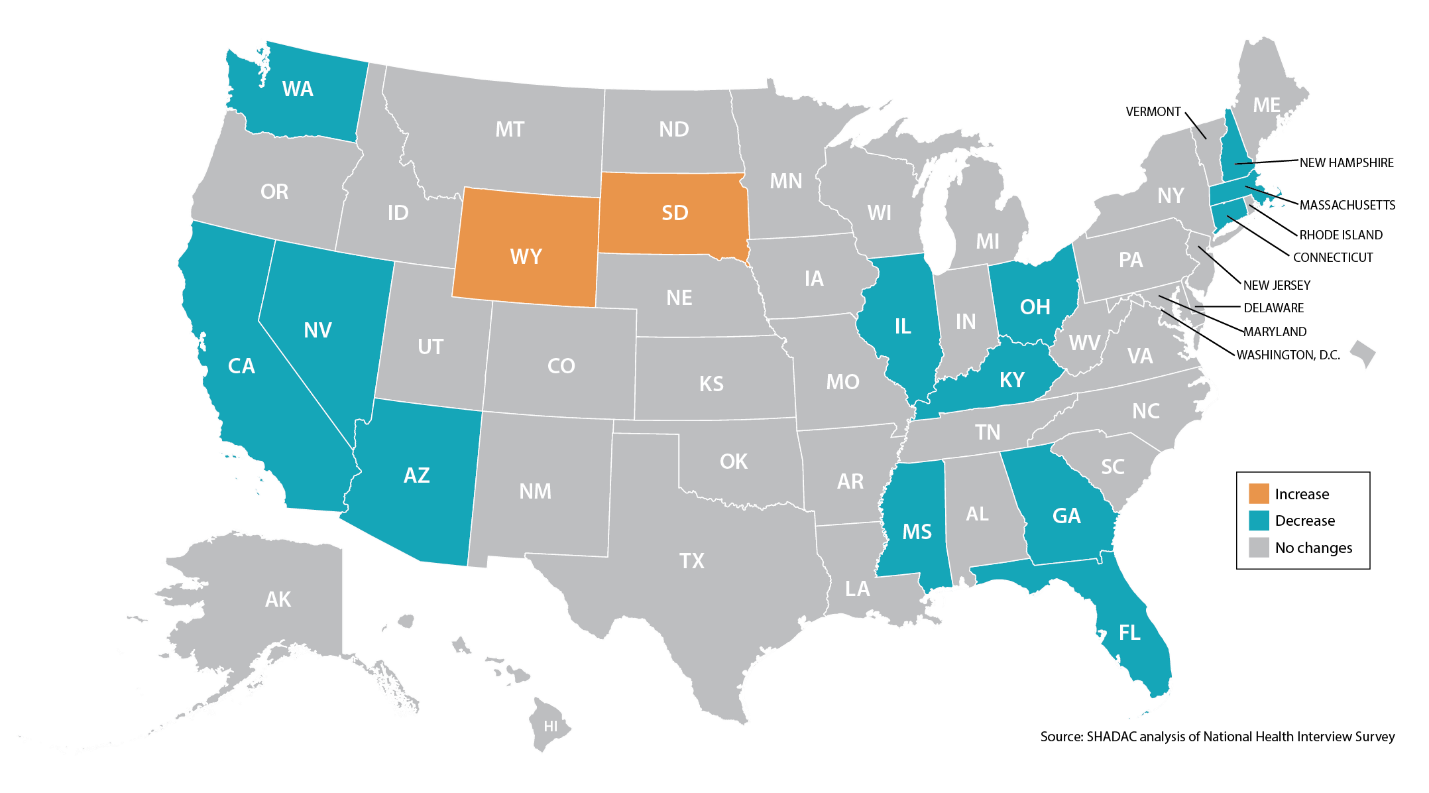
In addition to people with individual-market coverage, other groups also saw statistically significant reductions in rates of high-burden health spending. There was a 7.3 percentage point decline in high burden health spending among U.S. Medicare beneficiaries, from 33.6% in 2013 to 26.4% in 2015. At the same time, 24 states experienced statistically significant declines in rates of high-burden spending among Medicare beneficiaries (see Figure 1 below). Other evidence suggests those improvements may be the result of the ACA’s provision closing the Medicare Part D prescription drug “donut hole.”[ii],[iii] According to the U.S. Centers for Medicare & Medicaid Services, in 2015 Medicare beneficiaries saved $1,054 on average because of this ACA policy.[iv] Because the ACA gradually closes the donut hole until the gap is fully eliminated in 2020, it also will be important to continue monitoring high-burden spending among Medicare beneficiaries to assess whether Medicare beneficiaries continue to see reductions in high-burden spending.
Figure 1: Statistically Significant Changes in Medicare High-burden Spending, 2013-2015 (all ages)
The analysis also found a statistically significant decline of 1.5 percentage points (from 28.0% in 2013 to 26.5% in 2015) in the U.S. rate of high-burden spending among people with incomes from 0-400% of Federal Poverty Guidelines (FPG). This includes people eligible for the ACA’s Medicaid expansion (0-138% FPG) and people eligible for financial assistance to make individual-market coverage more affordable (139-400% FPG in Medicaid expansion states, and 100-400% FPG in non-expansion states). In contrast, rates of high-burden spending remained unchanged at 11.9% for people with incomes above 400% FPG, who weren’t eligible for the ACA’s Medicaid expansion or financial assistance.
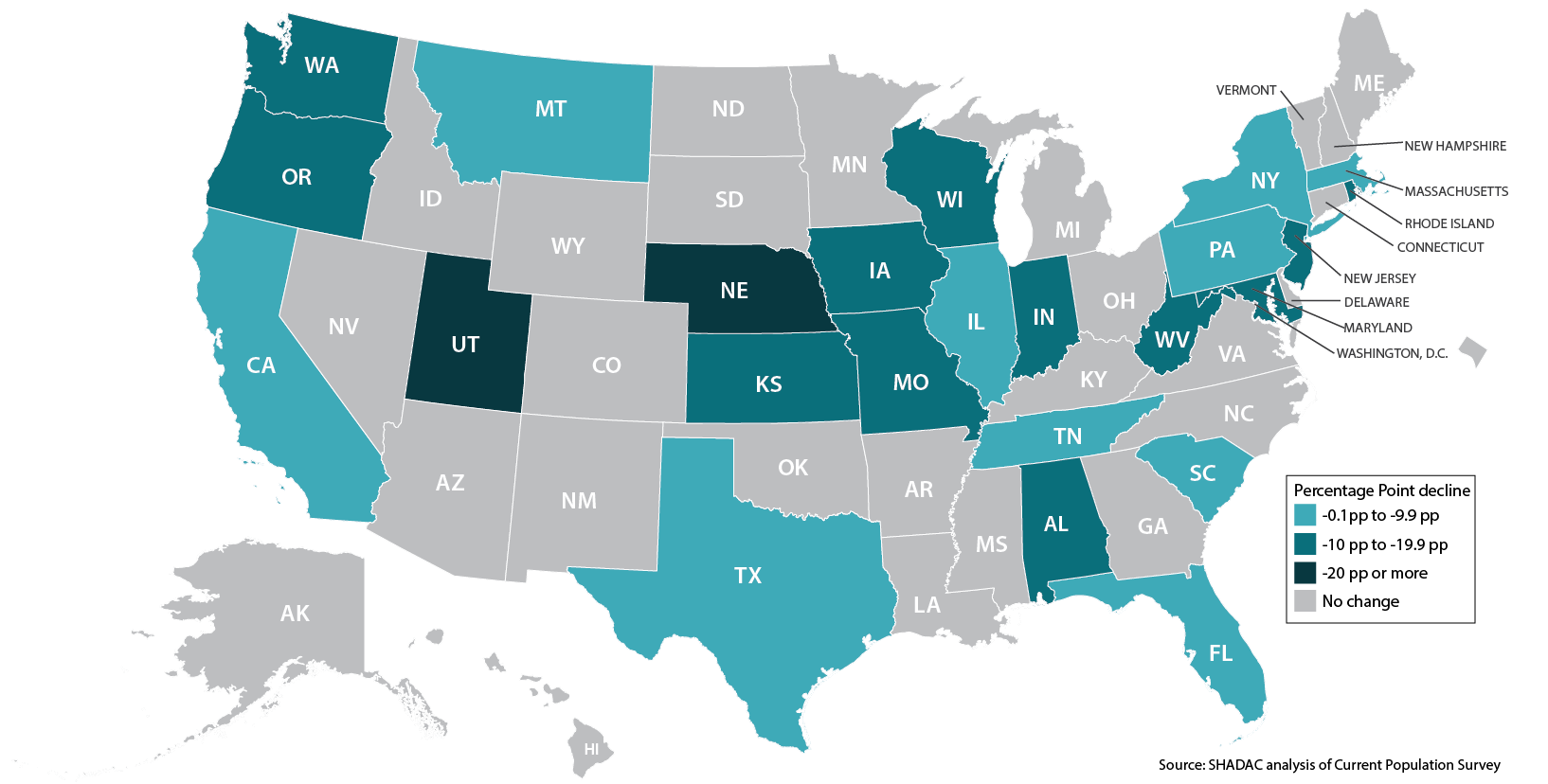
Other findings described in the brief include statistically significant declines in U.S. rates of trouble paying medical bills, and declines in rates of delayed and forgone care due to cost. Of the six states with significant changes in trouble paying medical bills, five saw improvements (California, Georgia, Montana, New Hampshire, North Dakota), while the share of Iowans reporting trouble paying medical bills increased. Of the 11 states with significant changes in delayed medical care due to cost, nine saw improvements (see Figure 2); and among the 15 states with significant changes in forgone care due to cost, 13 saw improvements (see Figure 3).
Overall, these findings suggest that the ACA may have reduced high-burden health care costs for individuals and families, especially for certain groups targeted by the law, such as people with individual-market coverage. Additionally, while few states experienced statistically significant changes, the significant changes in delayed and forgone care due to cost at the U.S. level suggest the ACA may be reducing cost-related barriers to care for some people.
Figure 2: Statistically Significant Changes in Rates of People Needing but Delaying Care Due to Cost, 2013-2015 (ages 0-64)
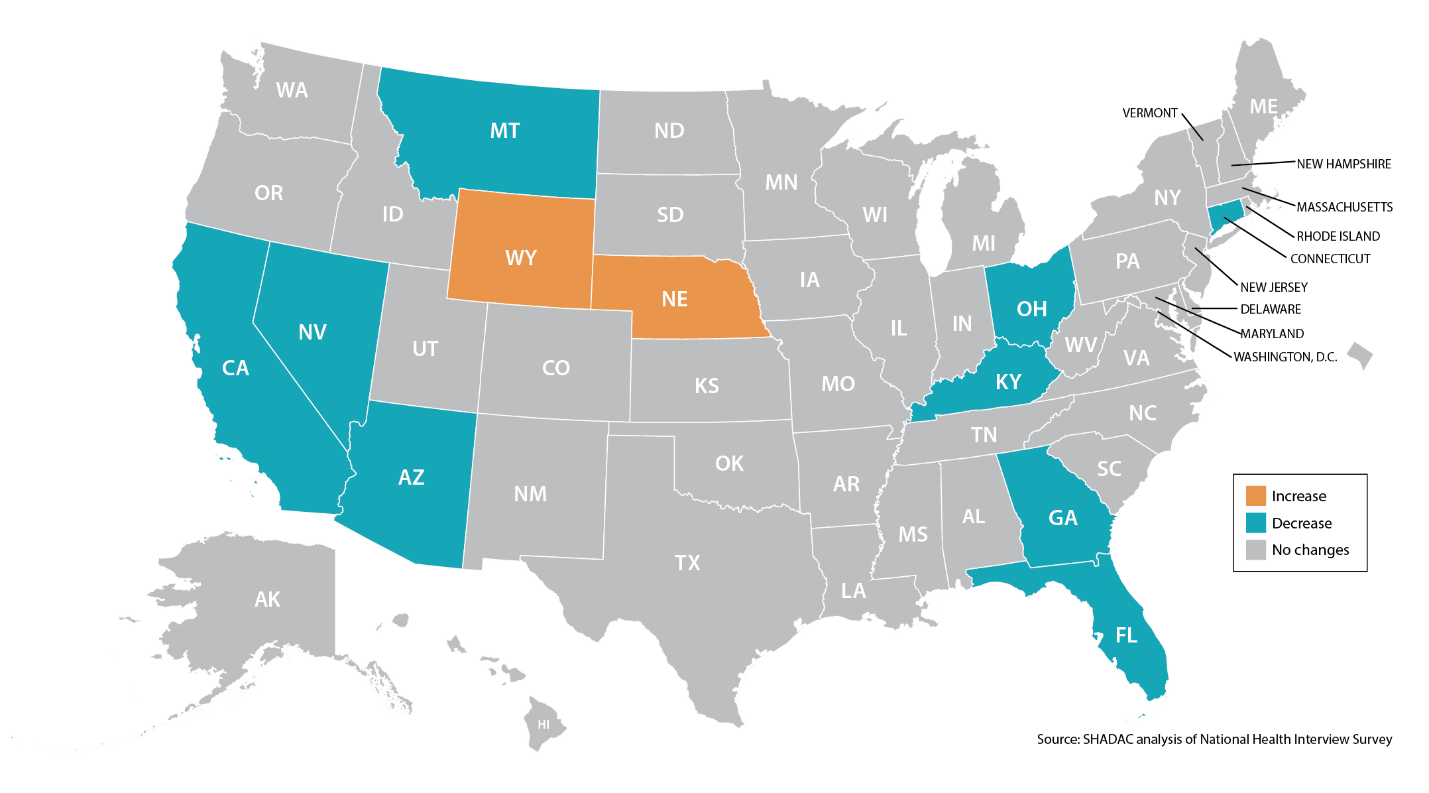
Figure 3: Statistically Significant Changes in Rates of People Needing but Going Without Care Due to Cost, 2013-2015 (ages 0-64)
[i] Volk, J., Palanker, D., Giovannelli, J., and Lucia, K. “Loss of Cost-Sharing Reductions in the ACA Marketplace: Impact on Consumers and Insurer Participation.” (2016). The Commonwealth Fund. Accessible at: http://www.commonwealthfund.org/publications/blog/2016/dec/loss-of-cost-sharing-reductions
[ii] Centers for Medicare & Medicaid Services (CMS). “More than 10 million people with Medicare have saved over $20 billion on prescription drugs since 2010.” (2016). Accessible at: https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2016-Press-releases-items/2016-02-08.html
[iii] CMS. “What is the Donut Hole?” (2010). Accessible at: https://blog.medicare.gov/2010/08/09/what-is-the-donut%C2%A0hole/
[iv] CMS. “Part D Donut Hole Savings by State 2015.” (Undated). Accessible at: https://downloads.cms.gov/files/Part%20D%20dount%20hole%20savings%20by%20state%20YTD%202015.pdf