Blog & News
New SHADAC Brief Explores National and State Estimates of Gains in Equitable Coverage for Mental Health and Substance Use Disorder under the ACA
July 09, 2019: A new brief from SHADAC, supported by the California Health Care Foundation (CHCF), examines gains in equitable coverage (i.e., “parity”) for mental health and substance use disorder (MH/SUD) treatment for people in the individual and small-group markets as well as those covered under Medicaid expansion after the passage of the Affordable Care Act (ACA). National and state-level estimates of parity gains for both types of treatment are provided within the brief, and estimates are broken down for the individual market, the small-group market, and the Medicaid expansion population.[1] These estimates provide important context for policymakers and others engaged in the ongoing debate about repealing, modifying, or replacing the ACA.
A new brief from SHADAC, supported by the California Health Care Foundation (CHCF), examines gains in equitable coverage (i.e., “parity”) for mental health and substance use disorder (MH/SUD) treatment for people in the individual and small-group markets as well as those covered under Medicaid expansion after the passage of the Affordable Care Act (ACA). National and state-level estimates of parity gains for both types of treatment are provided within the brief, and estimates are broken down for the individual market, the small-group market, and the Medicaid expansion population.[1] These estimates provide important context for policymakers and others engaged in the ongoing debate about repealing, modifying, or replacing the ACA.
Background
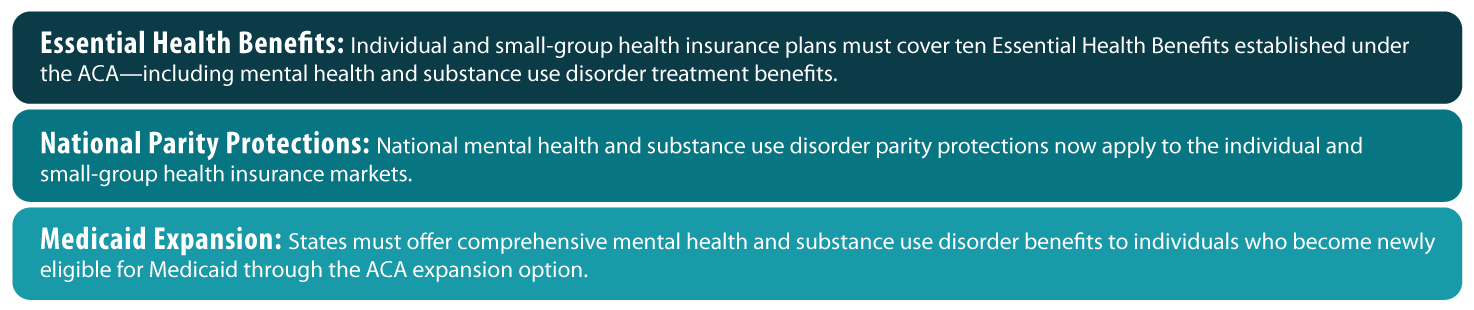
Before the ACA, national legislation regarding equitable coverage for MH/SUD treatments applied only to large-group (i.e., employer-sponsored) health plans, as a result of the Mental Health Parity Act of 1996 (MHPA) and the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA). The ACA extended these MH/SUD parity protections beyond the large-group market to the individual and small-group markets and to Medicaid expansion beneficiaries by making MH/SUD treatments an essential health benefit (EHB). Before this change, coverage and parity for MH/ SUD treatment in these markets were addressed unevenly across states through a patchwork of state laws.
Expanding Equitable Coverage of Mental Health and Substance Use Disorder Treatment under the ACA: Key Provisions
Findings
Mental Health
In total, an estimated 39 million individuals nationwide had health insurance that was subject to the ACA’s expanded MH parity requirements as of 2017. Of these, 12.1 million were enrolled in individual plans, 14.4 million were enrolled in small-group plans, and almost 13 million were newly eligible Medicaid expansion enrollees.
At the state level, California saw the greatest number of individuals affected at approximately 8.6 million. Other states that had high estimates of affected populations included New York with 2.1 million, Florida with 2.08 million*, Texas with 1.9 million*, and Pennsylvania with 1.87 million.
Vermont, which had pre-ACA parity in both the individual and small-group market and had expanded Medicaid in advance of the ACA, was the only state that saw no effect. Other states such as Wyoming*, Alaska, and Delaware, all had affected populations of less than 100,000 (44,000; 67,000; and 80,000, respectively).
Substance Use Disorder
In total, an estimated 36.4 million individuals nationwide had health insurance that was subject to the ACA’s expanded SUD parity requirements as of 2017. Of these, 9.8 million were enrolled in individual plans, 14 million were enrolled in small-group plans, and almost 12 million were newly eligible Medicaid expansion enrollees.
At the state level, California saw the greatest number of individuals affected at approximately 8.26 million, followed by New York (2.09 million), Florida* (1.79 million), Pennsylvania (1.79 million) and Texas* (1.7 million).
Massachusetts, which had pre-ACA parity in both the individual and small-group market and had expanded Medicaid in advance of the ACA, was the only state that saw no effect. Other states such as Delaware, Wyoming*, Maine*, and Alaska all had affected populations of less than 100,000 (12,000; 39,000; 52,000; and 64,000, respectively).
Discussion
Though the ACA mandated access to health insurance coverage with parity for treatment of mental health and substance use disorders for new groups, it is important to note that the expansion of coverage parity legislation does not guarantee access to equitable MH/SUD services unless the legislation is enforced. Responsibility for parity enforcement falls primarily to states, and the nature and extent of enforcement is consequently inconsistent across the country, with many parity violations continuing to occur as state regulators face limitations in their enforcement capacities.
Further Reading
Access and Cost Barriers to Mental Health Care, by Insurance Status, 1999-2010
Kathleen Rowan, Donna McAlpine, and Lynn Blewett
Section 1115 Waivers and ACA Medicaid Expansions: A Review of Policies and Evidence from Five States: May 2016
SHADAC Special Issue Brief
Medicaid Expansion: Comparing State Choices in Alternative Benefit Plan Design
Colin Planalp
To learn more about mental health and state-level estimates for the affected population who report mentally unhealthy days, see our recent blog post, and visit State Health Compare to learn more about the measure and its data sources.
[1] National estimates do not include a Medicaid expansion breakdown because expansion has only occurred at the state level.
* No Medicaid expansion