Blog & News
Lynn Blewett in Health Affairs Blog: Examining the New Basic Health Plan Financing Rule
October 2018:On August 24th, the Centers for Medicare and Medicaid (CMS) released a Final Administrative Order that would revise and recalculate their payments toward Basic Health Programs (BHPs). Only two states have established BHPs—Minnesota and New York—under Section 1331 of the Affordable Care Act (ACA).
SHADAC Director Lynn Blewett and David Anderson, a researcher at the Duke University Margolis Center, co-authored a Health Affairs blog that takes a look at the background of BHPs in Minnesota and New York, how this new order affects them, and what may happen with federal BHP financing going forward.
BHP Background and Financing
BHPs are optional state coverage programs designed to improve continuity of care and affordable coverage for low-income individuals who would otherwise be eligible for coverage on the health insurance Marketplace. Minnesota and New York both implemented BHPs in 2015, and their BHPs currently cover 89,000 and 700,000 people, respectively. BHPs must cover the ACA’s essential health benefits, and both New York and Minnesota offer low to no cost-sharing.
Federal funding for BHPs is based on 95 percent of the total advance premium tax credits (APTCs) and cost-sharing reductions that would have been provided if a state’s BHP population would have enrolled in the second-lowest-cost silver qualified health plan (QHP) on the state’s health insurance Marketplace. The methodology for determining payment is published annually and is based on BHP enrollment characteristics for each state, including age, geographic area, household size, and income. Minnesota estimated that approximately 25 percent of the federal funding for its BHP came from cost-sharing reductions.
Major Changes to BHP Federal Financing
In October 2017, the Centers for Medicare and Medicaid Services (CMS) announced it would stop paying cost-sharing reductions to insurers, who remain legally obligated to pay for these same reductions to cover costs of deductibles, coinsurance, and co-payments for individuals at 100 to 250 percent FPL in states that did not expand Medicaid, and 138 to 250 percent FPL in Medicaid expansion states. Many insurers chose to offset the elimination of cost-sharing reduction by increasing premiums in order to secure higher premium tax credits for consumers.
State and Federal Responses
Minnesota and New York were notified that the CMS would stop funding the cost-sharing reductions of their BHPs in December 2017, and payments were subsequently halted in the first quarter of 2018. Both Minnesota and New York initially requested that CMS revise its calculations to account for a higher premium tax credit component of BHP payments to make up for the cost-sharing elimination. CMS did not initially respond, and the states moved to sue CMS.
CMS responded to the litigation by providing an interim settlement of $169 million to the states and establishing a new BHP payment methodology that provides an 18.8 percent adjustment to the BHP payment for both Minnesota and New York based on a survey of health insurers on the extent of their 2018 premium increase attributed to the discontinuation of cost-sharing reduction funding. Both Minnesota and New York questioned the revised BHP payment methodology. However, the new methodology currently only holds for 2018, and it is yet unknown if it will be used to calculate payments for 2019 and 2020.
Learn More
Read the full Health Affairs blog to learn more about the future of BHPs for Minnesota and New York.
Blog & News
Now Available: SHADAC Presentations from the 2018 AcademyHealth Annual Research Meeting
July 19, 2018:SHADAC presentation materials from the 2018 AcademyHealth Annual Research Meeting (ARM) are now available. Click on the presentation titles below to view and download the materials.
- “The Intersection of Structural Risk Factors and Insurance-Based Discrimination on Healthcare Access Inequities”
Presenter: Kathleen Call
Co-Authors: Rhonda Jones-Webb, Brooke Cunningham, Giovann Alarcón, Sarah Hagge, Alisha Simon - “Who Gets It Right? Characteristics Associated with Accurate Reports of Health Insurance Coverage”
Presenter: Kathleen Call
Co-Authors: Angela Fertig, Joanne Pascale, Don Oellerich - “Minnesota LTSS Projection Model: MN-LPM”
Presenter: Giovann Alarcón
Co-Authors: Robert Hest, Lynn A. Blewett - “Modeling Financial Eligibility for Medicaid Payment of LTSS”
Presenter: Robert Hest
Co-Authors: Giovann Alarcón, Lynn A. Blewett - “Modeling State-based Reinsurance: One Option for Stabilization of the Individual Market"
Presenter: Brett Fried
Co-Authors: Lynn A. Blewett, Coleman Drake - “Advancements in Care Coordination: Findings from an Evaluation of Minnesota’s State Innovation Model Initiative”
Presenter: Carrie Au-Yeung
Co-Authors: Christina Worrall, Donna Spencer, Emily Zylla, Kelli Johnson, Lacey Hartman - “Section 1115 Medicaid Expansion Waivers: Implementation Experiences of Arkansas, Indiana, Iowa, & Michigan”
Presenter: Carrie Au-Yeung
Co-Authors: Emily Zylla, Elizabeth Lukanen, Colin Planalp
Blog & News
SHARE Panel at 7th Annual ASHEcon
July 30, 2018:The 2018 Conference of the American Society of Health Conomists (ASHEcon) will take place from June 10th to June 13th at Emory University in Atlanta, with this year's theme being "Economics and Public Health."
An ASHEcon panel featuring findings from recent SHARE-funded research projects is scheduled for Monday, June 11th, from 10:00 a.m. to 11:30 a.m. in the Azalea Room of the Emory Conference Center Hotel. Panel details are below.
Panel: Medicaid Eligibility Thresholds and Minimum Wage Laws: The Impact of State Policy Decisions on Health Insurance Coverage, Out-of-Pocket Spending, and Access to Care
Chair: Andrew Mulcahy (RAND Corporation)
Paper: Medicaid vs. Marketplace Coverage for Near-Poor Adults: Effects on Out-of-Pocket Spending and Coverage
Presenting Author: Fredric Blavin (Urban Institute)
Discussant: Andrew Mulcahy (RAND Corporation)
Paper: The Impact of Changes in Medicaid Eligibility Thresholds on Duration of Health Insurance Coverage and Access to Health Care
Presenting Author: Heather Dahlen (University of Minnesota)
Discussant: Marguerite Burns (University of Wisconsin - Madison)
Paper: Do Minimum Wage Changes Affect Employer-Sponsored Insurance Coverage?
Presenting Author: Christine Eibner (RAND Corporation)
Discussant: Thomas Buchmueller (University of Michigan)
Blog & News
Fifty-State Analysis Finds Lower Access to Care among Adults with Less Education
March 2018:A new analysis from SHADAC examines educational attainment and access to health care, looking at the extent to which adults (25 years and older) with different levels of education skipped needed care due to cost and did not have a personal doctor. These indicators are both available for all states in SHADAC’s State Health Compare.
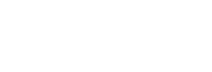
Skipping Needed Care Due to Cost
 The analysis, which uses data from the Behavioral Risk Factor Surveillance System (BRFSS), found that people with less education are much more likely to skip needed medical care for financial reasons: Nationally, adults with less than a high school education were more than three times as likely to skip care due to cost in 2016 than were adults with a bachelor’s degree or higher (22.9% vs. 7.3%). Among the states, all but one (Alaska[1]) saw significantly higher rates of foregone care among adults with less than a high school diploma than among college graduates. In seven states, the rate of foregone care among adults with less than a high school education exceeded the rate of foregone care among college graduates by more than 20 percentage points: Virginia, North Carolina, Alabama, Oklahoma, Arkansas, Georgia, and Nebraska.
The analysis, which uses data from the Behavioral Risk Factor Surveillance System (BRFSS), found that people with less education are much more likely to skip needed medical care for financial reasons: Nationally, adults with less than a high school education were more than three times as likely to skip care due to cost in 2016 than were adults with a bachelor’s degree or higher (22.9% vs. 7.3%). Among the states, all but one (Alaska[1]) saw significantly higher rates of foregone care among adults with less than a high school diploma than among college graduates. In seven states, the rate of foregone care among adults with less than a high school education exceeded the rate of foregone care among college graduates by more than 20 percentage points: Virginia, North Carolina, Alabama, Oklahoma, Arkansas, Georgia, and Nebraska.
The percentage of these adults with less than a high school diploma that skipped care due to cost has fallen nationally since the passage of the ACA, from 27.9% in the years preceding the ACA (2011 to 2013) to 24.1% in the years following the ACA (2014 to 2016). Among the states, 21 saw statistically significant declines in skipped care after the ACA, and none saw a significant increase.
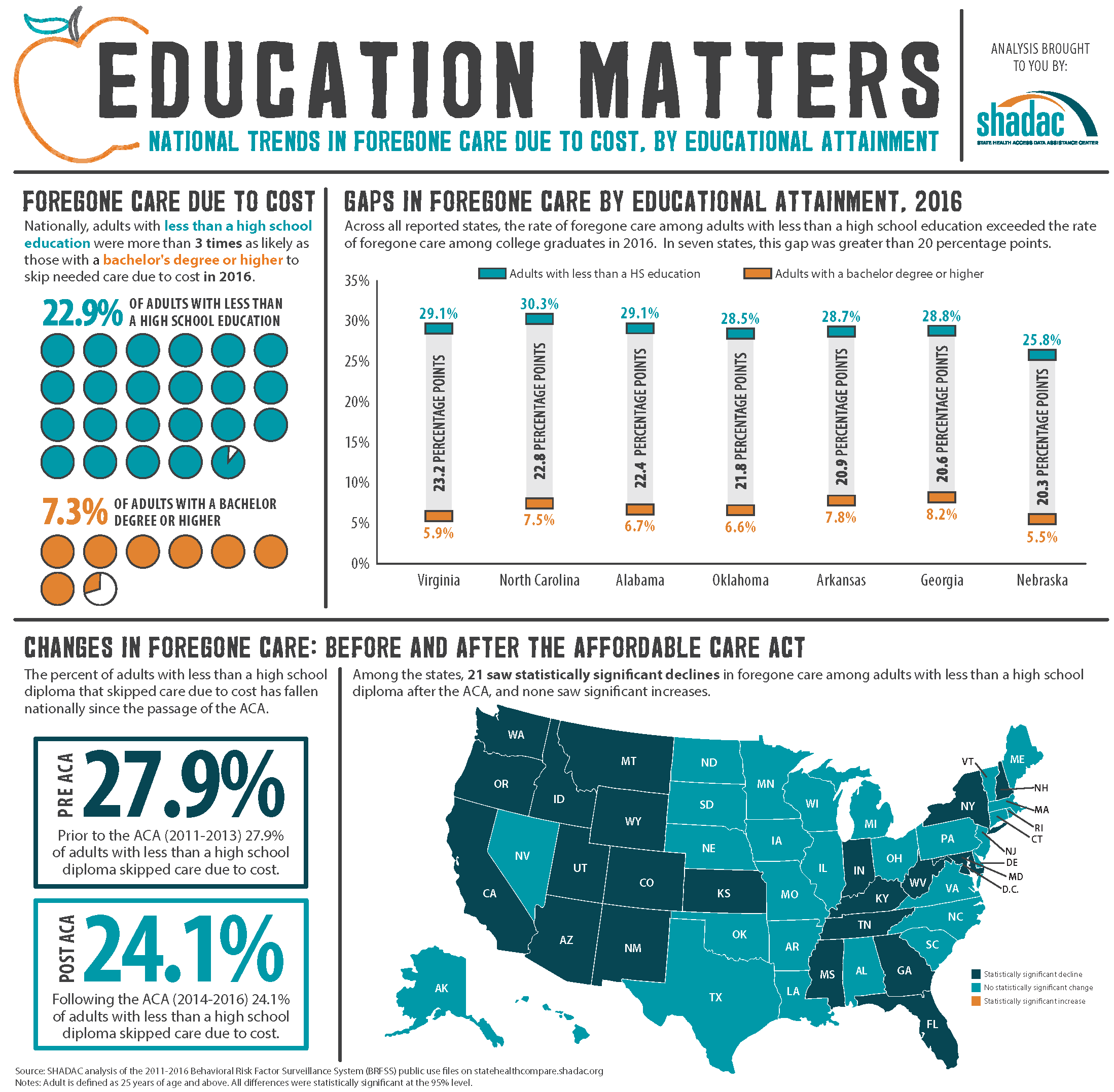
Not Having a Personal Doctor
 Nationwide, adults with less education were twice as likely to report that they did not have a personal doctor in 2016 as compared to people with a college degree or higher, at 31.8% vs. 15.2%. This same pattern was seen in 44 states. Among the remaining six states and the District of Columbia, no statistically significant differences were found between the two educational groups on reports of lacking a personal doctor. In ten states, the rate of not having a personal doctor among adults with less than a high school diploma exceeded the rate of not having a personal doctor among college graduates by more than 20 percentage points: Colorado, Wyoming, Kansas, Texas, Nevada, Utah, Georgia, Florida, Washington, and California.
Nationwide, adults with less education were twice as likely to report that they did not have a personal doctor in 2016 as compared to people with a college degree or higher, at 31.8% vs. 15.2%. This same pattern was seen in 44 states. Among the remaining six states and the District of Columbia, no statistically significant differences were found between the two educational groups on reports of lacking a personal doctor. In ten states, the rate of not having a personal doctor among adults with less than a high school diploma exceeded the rate of not having a personal doctor among college graduates by more than 20 percentage points: Colorado, Wyoming, Kansas, Texas, Nevada, Utah, Georgia, Florida, Washington, and California.
As with foregone care, the percentage of adults with less than a high school diploma who reported not having a personal doctor has fallen nationally since the enactment of the ACA, dropping from 33.8% to 31.9%. Significant declines on this measure were also seen in 7 states after the ACA went into effect, and 5 states saw significant increases.
States with More Adults Lacking a High School Diploma
Nationwide, 14.1% of adults had less than a high school diploma in 2016, and 16 states were above the national average on this measure. Texas, at 19.5%, had the highest percentage of adults with less than a high school diploma, followed by California (19.0%), Mississippi (18.0%), Louisiana (17.3%), and Kentucky (17.0%). North Dakota, New Hampshire, Wyoming, Montana, and Minnesota had the lowest percentages of residents with less than a high school education in 2016 (at 7.3%, 7.5%, 7.7%, 7.8%, and 7.9%, respectively).
State Fact Sheets
SHADAC researchers have created fact sheets for all states and the U.S. on the above measures. These fact sheets, along with infographics for select states, are available at www.shadac.org/Education&Access.
Learn More at State Health Compare
Learn more about the indicators used in this analysis, as well as other measures related to social determinants of health, at statehealthcompare.shadac.org.
[1] The 2016 estimate for this measure was suppressed for Alaska because the standard error is greater than 30% of the size of the estimate.
Publication
Section 1115 Medicaid Expansion Waivers: Implementation Experiences
This report summarizes SHADAC's analysis of how four states implemented Section 1115 Medicaid expansion wiavers. These states--Arkansas, Indiana, Iowa, and Michigan--are among eight that have expanded their Medicaid programs through Section 1115 of the Social Security Act rather than through the expansion option available under the Affordable Care Act (ACA).
 SHADAC's analysis was commissioned by the Medicaid and CHIP Payment and Access Commission (MACPAC) and sought to understan how Arkansas, Indiana, Iowa, and Michigan approached the implementation of key provisions of their Section 1115 Medicaid expansion waivers:
SHADAC's analysis was commissioned by the Medicaid and CHIP Payment and Access Commission (MACPAC) and sought to understan how Arkansas, Indiana, Iowa, and Michigan approached the implementation of key provisions of their Section 1115 Medicaid expansion waivers:
- Exchange plan premium assistance (Arkansas & Iowa)
- Enrollee contribution requirements (Iowa & Michigan)
- Health savings accounts (Arkansas & Indiana)
- Healthy behavior incentives (Indiana, Iowa, & Michigan)
- Graduated copayments for emergency department use (Indiana)
SHADAC researchers conducted interviews with 33 individuals representing current and former state agency staff and health insurance carriers in the four study states to identify the steps that states took to operationalize their programs. The report provides background information on the waiver program elements implemented in each of the four study states, summarizes the key pieces of administrative capacity that states put into place to implement their waivers, and details the specific program challenges they faced.