Publication
State Estimates of the Low-Income Uninsured Not Eligible for the ACA Medicaid Expansion
The Patient Protection and Affordable Care Act (ACA) will expand access to affordable health insurance for millions of Americans. In states that choose to implement the Medicaid expansion for low-income adults, Medicaid will provide an important new pathway to coverage. Yet, even in states that choose to expand Medicaid a significant proportion of the low-income nonelderly adult population will be excluded from the Medicaid expansion due to their immigration status. Legal permanent residents, in most circumstances, are ineligible for Medicaid benefits for the first five years during which they reside legally in the U.S. and unauthorized immigrants are excluded from Medicaid coverage. SHADAC Issue Brief #35 provides the first state-specific estimates of the number of uninsured low-income adults that will potentially be excluded from the Medicaid expansion because of their immigration status.
Blog & News
Disability Health Care Data and Information: Resources from SHADAC
July 24, 2024:- Unfair treatment in health care settings, at work, or when applying for public benefits
- Adults with disabilities are more likely to live in poverty compared to adults with no disability
- People with a disability often have increased medical expenses, with a study from the National Disability Institute estimating that a U.S. household containing an adult with a disability must spend an estimated 28% more income to obtain the same standard of living as a household with no disability
- Those with disabilities have twice the risk of developing chronic health conditions like depression, diabetes, asthma, and poor oral health
Federal Survey Sample Size Analysis: Disability, Language, and Sexual Orientation and Gender Identity
- People who indicated sexual orientation or gender identity (SOGI)
- People with language access needs, and
- People with disabilities
Collection of Self-Reported Disability Data in Medicaid Applications: A Fifty-State Review of the Current Landscape (SHVS Brief)
State Health Compare Disability Breakdowns
Housing Affordability Matters: Unaffordable Rents Infographics Updated with 2022 Data
Minnesota Community and Uninsured Profile
Stay Informed on Disability Health Data Resources and Information
Publication
Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination: Underlying Factors of Medicaid Inequities Annotated Bibliography
*Click here to jump to the 'Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination' annotated bibliography*
The State Health Access Data Assistance Center (SHADAC) with support from the Robert Wood Johnson Foundation (RWJF) and in collaboration with partner organizations is exploring whether a new national Medicaid Equity Monitoring Tool could increase accountability for state Medicaid programs to advance health equity while also improving population health.
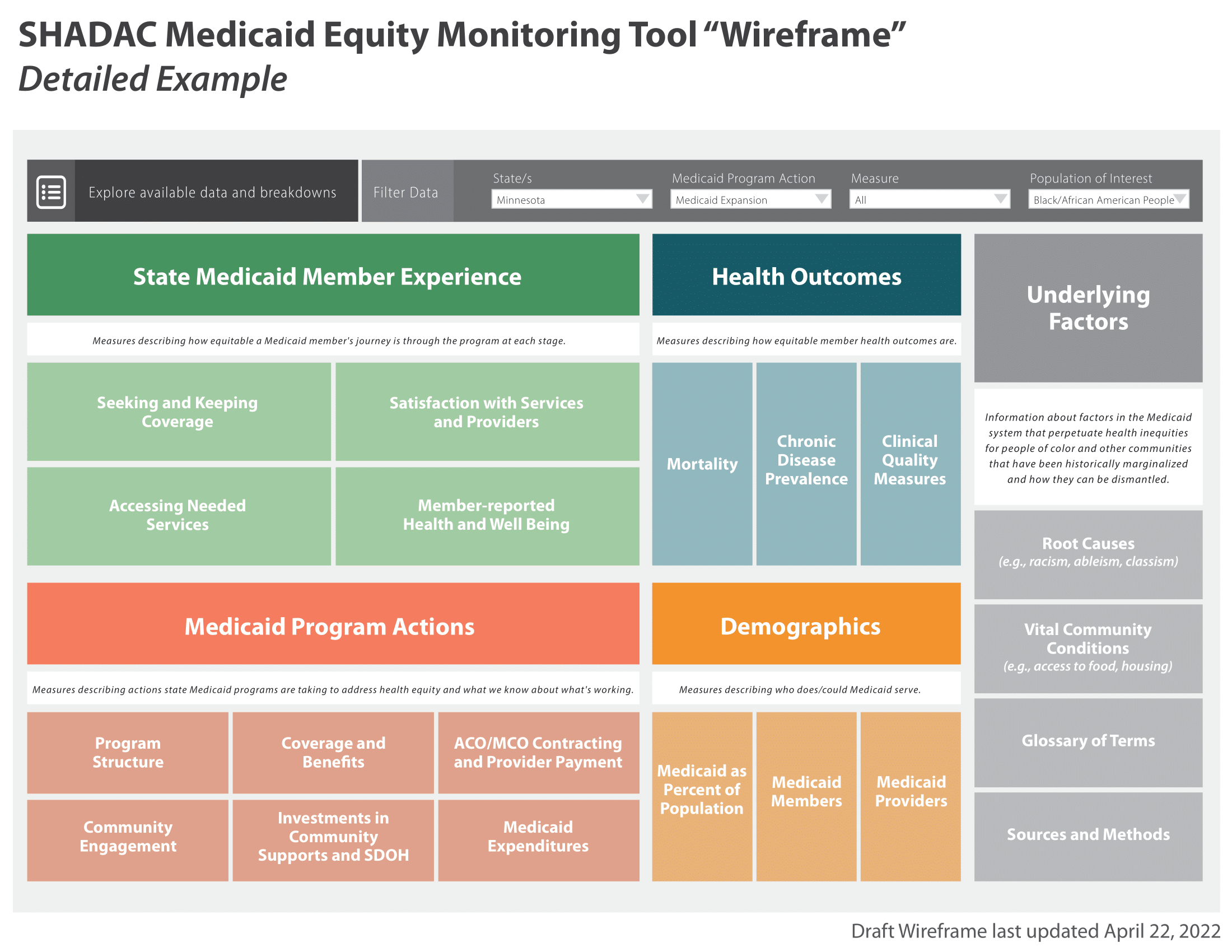
During the first phase of this project, a conceptual wireframe for the potential tool was created. This wireframe includes five larger sections, organized by various smaller domains, which would house the many individual concepts, measures, and factors that can influence equitable experiences and outcomes within Medicaid (see full wireframe below).
While project leaders and the Advisory Committee appointed at the beginning of the project all agree that the Medicaid program is a critical safety net, they specifically identified the importance and the need for an “Underlying Factors” section of the tool. This section aims to compile academic research and grey literature sources that explain and provide analysis for the underlying factors and root causes that may contribute to inequities in Medicaid.
 |
|
 |
- Historical context of Medicaid inequities
- Information on how underlying factors perpetuate inequities in Medicaid
- Potential solutions for alleviating inequities within Medicaid
Once selected, researchers compiled sources in an organized annotated bibliography, providing a summary of each source and its general findings. This provides users with a curated and thorough list of resources they can use to understand the varied and interconnecting root causes of Medicaid inequities. Researchers plan to continually update this curated selection as new research and findings are identified and/or released.
Sections of the full annotated bibliography include:
- Systemic Racism
- Systemic / Structural Ableism
- Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination
- Reproductive Oppression in Health Care (webpage forthcoming)
- Impact on Vital Community Conditions (webpage forthcoming)
This page is dedicated to a single section from the full annotated bibliography:
Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination

Underlying Factors Annotated Bibliography: Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination
Have a source you'd like to submit for inclusion in our annotated bibliography? Contact us here to propose a source for inclusion.
Click on the arrows to expand / collapse each source.
Mallory, C., & Tentindo, W. (2022). Medicaid Coverage for Gender-Affirming Care. Williams Institute UCLA School of Law. https://escholarship.org/content/qt4ng3j6st/qt4ng3j6st.pdf
Author(s): Christy Mallory and Will Tentindo, Williams Institute at University of California - Los Angeles
Article Type: Report
This report highlights key factors related to Medicaid coverage of gender affirming care. Emphasis is placed on the sheer number of individuals who identify as transgender or gender non-conforming that are covered by Medicaid – about one fourth of those who identify as transgender or gender non-conforming in the United States rely on Medicaid for their gender affirming care. Underlying factors contributing to inequities for this group include unclear language about what services are covered, and/or gender affirming care services are not covered at all in their state. Authors urge all states to fully expand their Medicaid program under the Affordable Care Act.
Kempf, R., Elias, N., & Rubin-DeSimone, A. (2021). Transgender and Gender Non-Binary Healthcare Coverage in State Medicaid Programs: Recommendations for More Equitable Approaches. Journal of Health and Human Services Administration, 44(1), 86–108. https://doi.org/10.37808/jhhsa.44.1.5
Author(s): Robin J. Kempf, Assistant Professor in the College of Public Service at the University of Colorado - Colorado Springs; Nicole M. Elias, Associate Professor in the Department of Public Management at John Jay College of Criminal Justice, City University of New York; Alonso J. Rubin-DeSimone, John Jay College of Criminal Justice, City University of New York
Article Type: Peer-reviewed journal
This peer reviewed journal article describes how transgender and gender non-binary individuals have been marginalized historically in U.S. society, including in terms of institutional or informal “erasure” as well as through isolation and “hypervisibility.” In health care, this discrimination translates into lack of access to qualified professionals and lack of coverage for a continuum of needed services. Authors chose to review state Medicaid program coverage policies to identify opportunities to build equity for all U.S. residents and noted that discrimination of individuals identifying as non-cisnormative gender can be compounded by the intersectionality of race, sexual orientation, socioeconomic status, and geographical location. They assessed comprehensiveness of state Medicaid coverage in accordance with the World Professional Association for Transgender Health (WPATH) standards. Authors found that the five states in their sample varied widely in terms of health coverage to transgender and gender non-binary Medicaid beneficiaries, however, there were stand out states in terms of the continuum of services offered as well as opportunities for improvement. Authors recommend removal of barriers to needed care such as prior authorization requirements as well as additional training for providers and individuals making coverage determinations.
Yuan, N., Chung, T., Ray, E. C., Sioni, C., Jimenez-Eichelberger, A., & Garcia, M. M. (2021). Requirement of mental health referral letters for staged and revision genital gender-affirming surgeries: An unsanctioned barrier to care. Andrology, 9(6), 1765–1772. https://doi.org/10.1111/andr.13028
Author(s): Nance Yuan, Cedars-Sinai Transgender Surgery and Health Program, and member of the Urology and Plastic Surgery Divisions at Cedars-Sinai Medical Center; Theodore Chung, David Geffen School of Medicine, University of California, Los Angeles; Alma Jimenez-Eichelberger and Caitlin Sioni, Cedars-Sinai Transgender Surgery and Health Program and the Division of Urology at Cedars-Sinai Medical Center; Edward C. Ray, Division of Plastic Surgery, Cedars-Sinai Medical Center; Maurice M. Garcia, Departments of Urology and Anatomy, University of California, San Francisco
Article Type: Peer-reviewed journal
This peer reviewed article investigates and discusses insurance requirements for referral letters from mental health providers prior to genital gender affirming surgeries for trans and non-binary individuals. In this study, half of the participants had federally funded insurance, such as Medicaid. Most plans, both public and private, required at least two referral letters at every stage of surgery (there may be four to five stages depending on the operation). Authors state that it took office staff, “an average of 2.5 hours per patient, per surgery, dedicated to coordinating submission of updated referral letters”. Some participants had to cancel or reschedule an operation due to lack of coordination of care, and/or administration not receiving referral letters. This resulted in patients being forced to pay for surgeries out-of-pocket instead of using insurance coverage. The authors discuss how multiple letters for each stage of a surgery is unnecessary, when no participant was deemed mentally unfit for any previously performed procedure. Authors state that requiring updated letters for each year was also a point of stress for participants as these administrative burdens were “costly and burdensome” to patients and providers alike. The authors urge organizations such as the World Professional Association for Transgender Health (WPATH) to revisit their recommendations for referral letter requirements to alleviate the burdens on both administrators and patients alike.
Mann, S. J., Carpenter, C. S., Gonzales, G., Harrell, B., & Deal, C. (2022). Effects of the affordable care Act’s Medicaid expansion on health insurance coverage for individuals in same-sex couples. Health Services Research, 58(3), 612–621. https://doi.org/10.1111/1475-6773.14128
Author(s): Samuel Mann, Christopher S. Carpenter, Benjamin Harrell, and Cameron Deal are all from the Department of Economics, LGBTQ+ Policy Lab, Vanderbilt University, Nashville, Tennessee; Gilbert Gonzales is also a member of the Department of Medicine, Health & Society, and Department of Health Policy at Vanderbilt University.
Article type: Peer-reviewed journal
This peer reviewed journal article analyzes how Medicaid expansion influenced health insurance coverage for individuals in same-sex partnerships. Using data from the American Community Survey, authors found that there was a significant increase in coverage between 2009 and 2018 for low-income adults who were in a same-sex relationship, especially for women. The authors attribute this to a much higher prevalence of children being in households of women same-sex couples compared to men. The authors also state that sexual minority women may have stronger social ties that reduce stigma surrounding Medicaid or public options compared to sexual minority men. This research has implications that are important for policymaking and underlying factors of inequity within Medicaid in terms of barriers to seeking health insurance coverage and accessibility of services for those individuals in same-sex partnerships.
[1] Human Rights Campaign. (n.d.). Sexual Orientation and Gender Identity Definitions. Human Rights Campaign; HRC Foundation. https://www.hrc.org/resources/sexual-orientation-and-gender-identity-terminology-and-definitions
[2] Ibid.
[3] HHS Office of Population Affairs. (n.d.). Gender-Affirming Care and Young People. U.S. Department of Health & Human Services. https://opa.hhs.gov/sites/default/files/2023-08/gender-affirming-care-young-people.pdf
Blog & News
LGBT Health Equity: Sexual Orientation and Gender Identity Data Resources and Information from SHADAC
July 02, 2024:- Less likely to have health insurance coverage
- Less likely to have a regular health care provider
- More likely to delay care
- More likely to report poor quality care and unfair treatment from providers
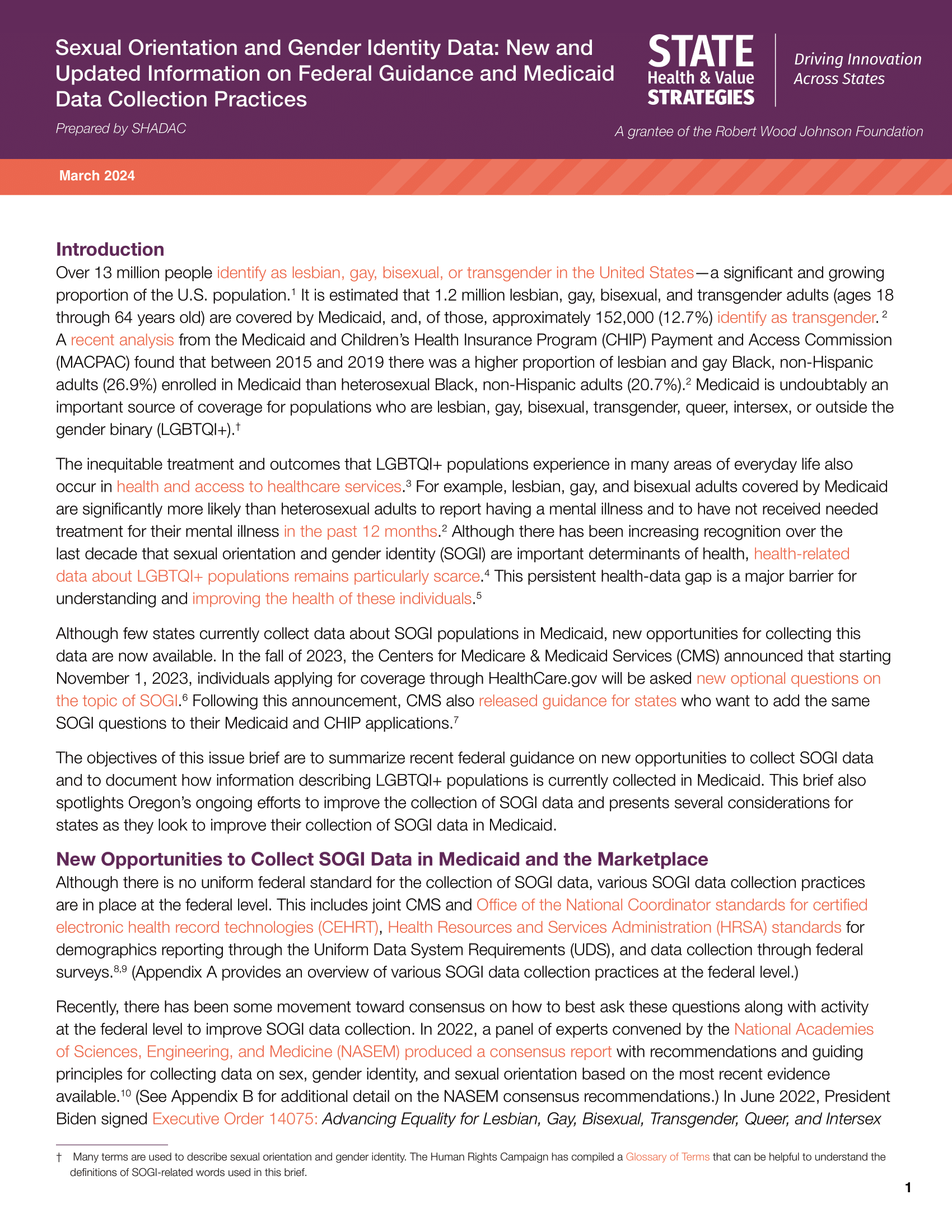
Sexual Orientation and Gender Identity Data: New and Updated Information on Federal Guidance and Medicaid Data Collection Practices (SHVS Brief)
State Health Compare: Explore Health Data with SOGI Data Breakdowns
- Adults Who Forgo Needed Medical Care Due to Cost
- Adult Smoking
- Adult Excessive Alcohol Consumption
- Adult E-Cigarette Use
- Chronic Disease Prevalence
- Adult Unhealthy Days
- Activities Limited Due to Health Difficulty
- Adults with No Personal Doctor
- Adult Cancer Screenings
- Adult Flu Vaccinations
Gender Based Discrimination in Health Care by Gender Identity in Minnesota
- Over half (57.1%) of trans and non-binary people reported forgone care—more than double the overall average of 26.2%
- Nearly one-third of trans and non-binary adults had low confidence in getting necessary health care—compared to the overall average of 11.8%
Examining Discrimination and Health Care Access by Sexual Orientation in Minnesota
- Both lesbian/gay and bisexual/pansexual people were more likely to report barriers to health care access
- Bisexual/pansexual people were more likely to report having low confidence in the ability to get needed health care
- Both lesbian/gay or bisexual/pansexual people had significantly higher rates of forgone care
SHADAC Response to 2023 Request for Comments on American Community Survey SOGI Questions
Stay Up to Date on the Latest in SOGI and LGBT Health Data
Publication
Underlying Factors of Medicaid Inequities Annotated Bibliography: Systemic / Structural Ableism
*Click here to jump to the 'Systemic Ableism' annotated bibliography*
The State Health Access Data Assistance Center (SHADAC) with support from the Robert Wood Johnson Foundation (RWJF) and in collaboration with partner organizations is exploring whether a new national Medicaid Equity Monitoring Tool could increase accountability for state Medicaid programs to advance health equity while also improving population health.
During the first phase of this project, a conceptual wireframe for the potential tool was created. This wireframe includes five larger sections, organized by various smaller domains, which would house the many individual concepts, measures, and factors that can influence equitable experiences and outcomes within Medicaid (see full wireframe below).
While project leaders and the Advisory Committee appointed at the beginning of the project all agree that the Medicaid program is a critical safety net, they specifically identified the importance and the need for an “Underlying Factors” section of the tool. This section aims to compile academic research and grey literature sources that explain and provide analysis for the underlying factors and root causes that may contribute to inequities in Medicaid.
 |
|
 |
- Historical context of Medicaid inequities
- Information on how underlying factors perpetuate inequities in Medicaid
- Potential solutions for alleviating inequities within Medicaid
Once selected, researchers compiled sources in an organized annotated bibliography, providing a summary of each source and its general findings. This provides users with a curated and thorough list of resources they can use to understand the varied and interconnecting root causes of Medicaid inequities. Researchers plan to continually update this curated selection as new research and findings are identified and/or released.
Sections of the full annotated bibliography include:
- Systemic Racism
- Systemic / Structural Ableism
- Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination
- Reproductive Oppression in Health Care (webpage forthcoming)
- Impact on Vital Community Conditions (webpage forthcoming)
This page is dedicated to a single section from the full annotated bibliography:
Systemic Ableism

Underlying Factors Annotated Bibliography: Systemic / Structural Ableism
Have a source you'd like to submit for inclusion in our annotated bibliography? Contact us here to propose a source for inclusion.
Click on the arrows to expand / collapse each source.
Friedman, C., & VanPuymbrouck, L. (2019). The relationship between disability prejudice and Medicaid home and community-based services spending. Disability and Health Journal, 12(3), 359–365. https://doi.org/10.1016/j.dhjo.2019.01.012
Author(s): Carli Friedman, Director of Research for The Council on Quality and Leadership (CQL) at the University of Washington; Laura VanPuymbrouck, Assistant Professor of Occupational Therapy at Rush University
Article Type: Peer-reviewed journal
This peer reviewed article summarizes findings from a quantitative study exploring the association between ableism in the U.S. and Medicaid spending on long term services and supports. It begins with historical context about deinstitutionalization of people with disabilities and the history of Medicaid as both a primary payer for long-term care and an insurer for people with disabilities. Despite research indicating community living has more benefits than institutions, investments in home and community-based services vary state to state; authors hypothesize that an association exists between stereotypical attitudes toward people with disabilities (i.e., as dependent, a drain, not capable) and state decision making. Using CMS expenditure data and survey data from the Disability Attitudes - Implicit Association Test, authors found a negative association between state prejudice scores and state funding of home health and community-based services. While causality cannot be assumed, authors conclude by stressing the importance of understanding how disability prejudice is embedded into our society, and how it may influence Medicaid and other policy decisions. These findings are a call to advocate for increased investment in community services and to promote advocacy for the health and well-being of people with disabilities.
Earl, E. (2023). Promoting Health Care Equity: The Instrumentality of Medicare and Medicaid in Fighting Ableism Within the American Health Care System. Seton Hall Law Review: Vol. 53: Iss. 5, Article 9. Available at: https://scholarship.shu.edu/shlr/vol53/iss5/9
Author(s): Emmalise Earl, Seton Hall University, Judicial Law Clerk in New Jersey Court System
Article Type: Peer-reviewed journal
This article discusses long-standing systemic issues with having accessible health care tools and equipment for people with physical disabilities. Despite the passage of the American Disabilities Act in 1973, which requires hospitals and clinics to have physically accessible equipment for care for all individuals regardless of mobility status, the Act has gone loosely enforced for decades according to the author. Lack of accessible equipment for routine checkups, such as scales and exam tables, results in incomplete examinations, later and more severe diagnoses due to inability to screen those with mobility related disabilities, as well as an exacerbation of current diagnoses due to incomplete or less effective treatment. The author states that “without more aggressive enforcement, these circumstances are not likely to change”. The author uses the Department of Veterans Affairs (VA) hospitals as an exemplar for what is needed to uphold accessibility standards. The VA requires all new medical equipment to be approved as accessible by their Access Board. The author also describes specific program actions that the Center for Medicare and Medicaid Services needs to take in enforcing equitable access to medical equipment. For Medicaid in particular, the author suggests that state Medicaid agencies adopt and enforce standards that facilities and providers must follow in order to participate in the Medicaid program. The authors also suggest leveraging tax incentives to overcome financial barriers to accessibility.
Valdez, R. S., & Swenor, B. K. (2023). Structural Ableism — Essential Steps for Abolishing Disability Injustice. The New England Journal of Medicine, 388(20), 1827–1829. https://doi.org/10.1056/nejmp2302561
Author(s): Rupa S. Valdez, the Departments of Public Health Sciences and Engineering Systems and Environment, University of Virginia; and Bonnielin Swenor, the Disability Health Research Center, Bloomberg School of Public Health, Johns Hopkins University
Article Type: Peer-reviewed journal perspective
This article discusses the details of systemic ableism and its effects on those with intellectual and/or physical disabilities. The authors maintain that this underlying factor of health inequities is often ignored in health care and research spaces. In addition, more attention is needed on the ways structural ableism interacts with other forms of oppression. The core purpose of this article is to highlight achievable and actionable solutions for alleviating bias and discrimination of those with disabilities. Proposed solutions include establishing measures of structural ableism within research and providing accessibility options within physical environments (e.g. streets & roadways, buildings, neighborhoods, and cities). The authors also emphasize a need for the adaptation of measures of structural racism plus the addition of new measurement domains. Of particular importance for the authors is measuring both the funding allocated for home and community based services within the Medicaid program as well as measuring the rate of violations of the Olmstead decision, which entitles those with disabilities to community integration and community-based services. Consideration of qualitative methods and community partnership in this work is also crucial for creating actionable and effective solutions to issues of systemic ableism.
[1] Valdez, R. S., & Swenor, B. K. (2023). Structural Ableism — Essential Steps for Abolishing Disability Injustice. The New England Journal of Medicine, 388(20), 1827–1829. https://doi.org/10.1056/nejmp2302561